Page last updated: December 2024
The information on this webpage was adapted from Understanding Peripheral Neuropathy and Cancer - A guide for people affected by cancer (2024 edition). This webpage was last updated in December 2024.
Expert content reviewers:
This information was developed with the help of a range of health professionals and people affected by peripheral neuropathy:
- Dr Fiona Day, Senior Staff Specialist Medical Oncologist, Calvary Mater Newcastle, NSW
- James Chirgwin, Senior Physiotherapist – Oncology, Haematology and Palliative Care, The Wesley Hospital, QLD
- Kim Kerin-Ayres, Nurse Practitioner Cancer Survivorship, Sydney Cancer Survivorship Centre, Concord Hospital, NSW
- Melanie Moore, Lead Exercise Physiology Clinical Supervisor, UC Cancer Wellness Clinic, University of Canberra, ACT
- Olivia Palac, Acting Assistant Director, Occupational Therapy, Gold Coast University Hospital, QLD
- Danielle Rippin, Consumer
- Dr Jane Wheatley, Clinical and Health Psychologist, Department of Pain Medicine, St Vincent’s Health Network, Sydney, NSW
What is peripheral neuropathy?
Peripheral neuropathy is damage to the peripheral nerves. These nerves carry information between the central nervous system (brain and spinal cord) and the rest of the body.
Unlike many other cells in the body, nerve cells aren’t easily repaired or replaced once they are badly damaged. Cancer, or some cancer treatments, can cause peripheral neuropathy. It can also happen due to an accident or injury, infection or diabetes.
The symptoms can vary, and depend on which type of peripheral nerves are affected.
Peripheral neuropathy most often affects the hands or feet with feelings of numbness, pain or burning, a loss of sensation, tingling or “pins and needles”. If the condition worsens, these symptoms may start to spread further up the arms and legs.
Other symptoms may include muscle weakness, cramping, dizziness, balance issues, trouble sensing where your feet or hands are, ringing in the ears (tinnitus), hearing loss or constipation.
Symptoms range from mild to severe, appear during or after treatment and can be temporary or permanent (or last for months or years).
The symptoms may be worse at night and disrupt sleep, and can greatly affect quality of life – but there are often ways to help manage changes.
About the nervous system
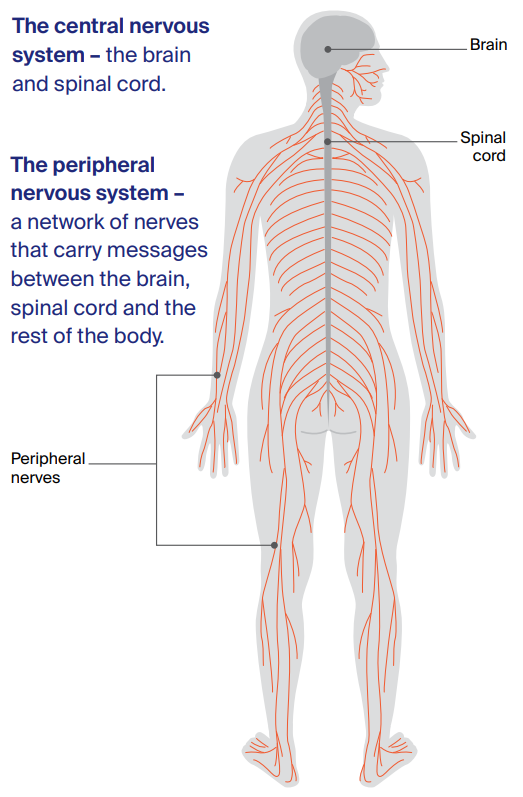
The nervous system controls everything your body does. It has two main parts:
- central nervous system – the brain and spinal cord
- peripheral nervous system – a network of nerves that carry messages between the brain, spinal cord and the rest of the body.
How nerves work
Nerves are made up of nerve cells called neurons. When a nerve ending in the body (for example, in the finger) is stimulated, a tiny electrical signal is sent through the neuron and nerve system to the spinal cord and brain.
If a peripheral nerve is damaged, the electrical signals may be changed, blocked or mixed up, leading to a wide range of symptoms.
What causes peripheral neuropathy?
There are many causes of peripheral neuropathy. Some types of chemotherapy used to treat cancer may damage peripheral nerves. This side effect is called chemotherapy-induced peripheral neuropathy (CIPN).
Sometimes, other treatments such as immunotherapy, or the cancer itself, are the cause. Possible cancer-related causes of peripheral neuropathy include:
- certain chemotherapy drugs, in particular taxanes (e.g. docetaxel, paclitaxel), platinum drugs (e.g. carboplatin, cisplatin, oxaliplatin) and vinca alkaloids (e.g. vincristine)
- the use of immunotherapy drugs
- some other cancer drugs, such as thalidomide, bortezomib and brentuximab vedotin
- some types of cancer (e.g. lung cancer, myeloma and lymphoma)
- tumours pressing on nerves
- surgery or radiation therapy damaging nerves.
Diabetes, shingles, heavy use of alcohol and some drugs, and a lack of certain vitamins and minerals (especially vitamin D and some B vitamins) can also cause, or contribute to, your risk of peripheral neuropathy. Smoking may also increase your risk.
Will I get it if I have chemotherapy?
About 40% of people who have chemotherapy will have symptoms of peripheral neuropathy, but the risk varies with different chemotherapy drugs.
In people treated with certain chemotherapy drugs, the rate is higher, with about 70% of these people experiencing some symptoms a month after treatment, and about 30% still having symptoms 6 months after treatment finishes.
Can it be prevented?
So far, no therapy has been proven to prevent peripheral neuropathy, although studies suggest that exercise may help.
Researchers are studying whether ice mitts and booties (gloves and socks) worn during chemotherapy could help, but there is not enough evidence yet to tell if this works.
It may help to be checked for any existing nerve damage before starting treatment, so that any changes can be checked against this baseline.
If you start having symptoms during chemotherapy treatment, your doctor may reduce the doses of chemotherapy drugs, or increase the time between treatment cycles. This sometimes allows the nerves to recover and prevents permanent damage.
Some people may need to stop having a particular chemotherapy drug. You can talk to your doctor about how they will balance the risk of changing the chemotherapy plan against the risk of the nerve damage becoming permanent.
If you have diabetes, it should be managed well and blood sugar levels monitored carefully, to lower your risk of peripheral neuropathy. Limiting the amount of alcohol you drink, staying a healthy weight and not smoking may also lower your risk.
Talk to your treatment team about your individual risk factors, including medicines that may increase your risk.
Will it get better?
Some types of chemotherapy cause short (acute) episodes of peripheral neuropathy during, or soon after, a cancer treatment session. These episodes tend to last a few days.
For other types of chemotherapy, peripheral neuropathy may be longer-lasting (chronic). It may start during treatment and the risk increases the more treatment cycles that you have.
In some cases, peripheral neuropathy can develop or get worse over time, even after treatment has finished. The peripheral neuropathy symptoms may begin to improve over 6–12 months.
In some people, symptoms are permanent and may be mild to severe. This is more likely if you have had intensive treatment, such as a high-dose chemotherapy, or if you have diabetes or other risk factors.
Driving safely
Ask your doctor if it’s safe to drive or operate machinery, especially if you do this for work.
Depending on the symptoms, you may need a break from driving and your licence may be impacted.
Understanding Peripheral Neuropathy and Cancer
Download our Understanding Peripheral Neuropathy and Cancer fact sheet to learn more
Download now