Page last updated: October 2024
The information on this webpage was adapted from Understanding Lung Cancer - A guide for people with cancer, their families and friends (2024 edition). This webpage was last updated in October 2024.
Expert content reviewers:
This information was developed based on Australian and international clinical practice guidelines, and with the help of a range of health professionals and people affected by lung cancer:
- Dr Malinda Itchins, Thoracic Medical Oncologist, Royal North Shore Hospital and Chris O’Brien Lifehouse, NSW
- Dr Cynleen Kai, Radiation Oncologist, GenesisCare, VIC
- Dr Naveed Alam, Thoracic Surgeon, St Vincent’s Hospital, Epworth Richmond, and Monash Medical Centre, VIC
- Helen Benny, Consumer
- Dr Rachael Dodd, Senior Research Fellow, The Daffodil Centre, NSW
- Kim Greco, Specialist Lung Cancer Nurse Consultant, Flinders Medical Centre, SA
- Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA
- Marco Salvador, Consumer
- Janene Shelton, Lung Foundation Australia – Specialist Lung Cancer Nurse, Darling Downs Health, QLD
- Prof Emily Stone, Respiratory Physician, Department of Thoracic Medicine and Lung Transplantation, St Vincent’s Hospital Sydney, NSW
- A/Prof Marianne Weber, Stream Lead, Lung Cancer Policy and Evaluation, The Daffodil Centre, NSW.
What is lung cancer?
Lung cancer begins when abnormal cells grow and multiply in an uncontrolled way in one or both lungs.
Cancer that starts in the lungs is known as primary lung cancer. It can spread to other parts of the body such as the lymph nodes, pleura, brain, adrenal glands, liver and bones.
When cancer spreads to the lungs from another part of the body (e.g. breast or bowel), this is known as secondary or metastatic lung cancer. This information is about primary lung cancer only.
How common is lung cancer?
Each year, about 15,500 Australians are diagnosed with lung cancer. The average age at diagnosis is 72 years.
More men than women develop lung cancer, but since the early 1980s rates have been steadily decreasing among men and increasing among women.
More lung cancer statistics and trends
The lungs
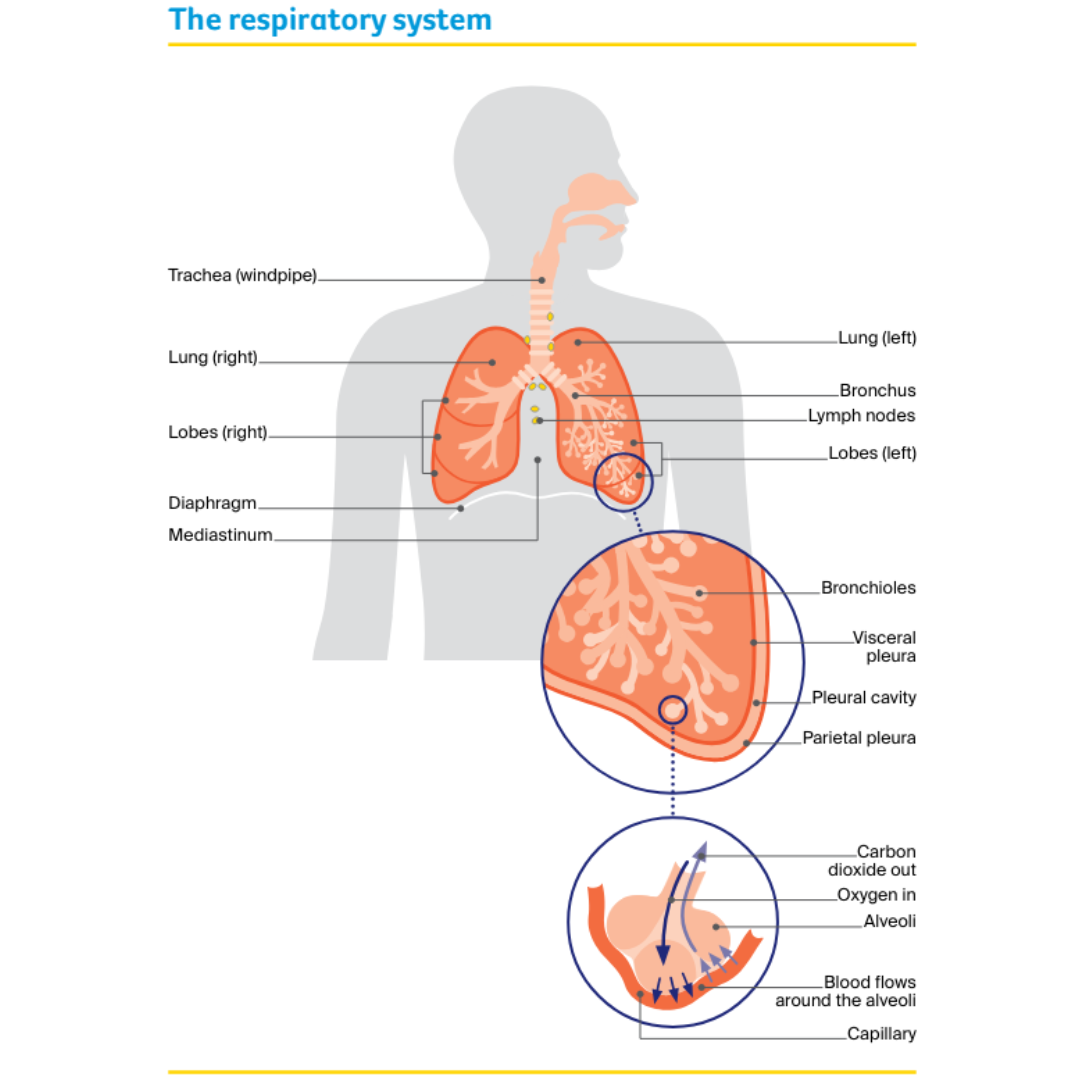
The lungs are two sponge-like organs that are used for breathing. They are part of the respiratory system, which also includes the nose, mouth, trachea (windpipe) and airways (tubes) to each lung.
There are large airways known as bronchi (singular: bronchus) and small airways called bronchioles. The lungs sit in the chest and are protected by the rib cage.
Lobes
Each lung is made up of sections called lobes – the left lung has two lobes, and the right lung has three lobes.
Diaphragm
The lungs rest on the diaphragm, which is a wide, thin muscle that helps with breathing, and separates the chest from the abdomen (belly).
Mediastinum
The space between the lungs is called the mediastinum. A number of important structures lie in this space, including:
- the heart and large blood vessels
- the trachea – the tube that carries air into the lungs
- the oesophagus – the tube that carries food to the stomach
- lymph nodes – small, bean-shaped structures that collect and destroy bacteria and viruses.
Pleura
The lungs are covered by two thin layers of tissue called the pleura. The inner layer (visceral pleura) lines the lung surface, and the outer layer (parietal pleura) lines the chest wall, mediastinum and diaphragm.
The layers are separated by a small amount of fluid that lets them smoothly slide over each other when you breathe. The pleural cavity is the potential space between the two layers; there is no space between the layers when the lungs are healthy.
How breathing works
When you breathe in (inhale), your diaphragm moves down and air goes down the trachea and into the bronchi and bronchioles.
When the inhaled air reaches the tiny air sacs called alveoli, oxygen passes through the small blood vessels (capillaries) and into the blood.
When you breathe out (exhale), your diaphragm relaxes and moves back up, and a waste gas called carbon dioxide is removed from the body and released into the air.
Your guide to best cancer care
A lot can happen in a hurry when you’re diagnosed with cancer. The guide to best cancer care for lung cancer can help you make sense of what should happen.
It will help you with what questions to ask your health professionals to make sure you receive the best care at every step.
Read the guide
Types of lung cancer
There are two main types of primary lung cancer: non-small cell lung cancer and small cell lung cancer.
Pleural mesothelioma is a type of cancer that affects the covering of the lung (the pleura). It is different from lung cancer and is usually caused by exposure to asbestos.
Other types of cancer, like cancers that start in the chest wall, and lung diseases such as silicosis may also affect the lungs and have similar symptoms but are not considered lung cancer.
Non-small cell lung cancer (NSCLC)
NSCLC makes up about 85% of lung cancers. It may be classified as:
- adenocarcinoma – begins in mucus-producing cells, more often found in the outer part of the lungs.
- squamous cell carcinoma – begins in thin, flat cells, most often found in the larger airways.
- large cell undifferentiated carcinoma – the cancer cells are not clearly squamous or adenocarcinoma.
Small cell lung cancer (SCLC)
SCLC makes up about 15% of lung cancers. It tends to start in the middle of the lungs, and usually spreads more quickly than NSCLC.
Risk factors for lung cancer
A risk factor is anything that increases a person’s chances of developing a certain condition, such as cancer. It is possible to avoid or reduce the impact of some risk factors. Some people develop lung cancer without having any risk factors.
The following factors are known to increase the risk of lung cancer. This does not mean you will develop lung cancer, but if you are concerned, talk to your doctor.
Tobacco smoking factors
Most cases of lung cancer are caused by tobacco smoking. The earlier a person starts smoking, the longer they smoke and the more they smoke, the higher their risk of developing lung cancer.
People who have never smoked can also get lung cancer. About 15% of cases occur in men who have never smoked, and about 30% of cases occur in women who have never smoked.
Quit smoking
Environmental or work-related factors
- Second-hand smoking – Breathing in other people's tobacco smoke (second-hand smoke) may cause lung cancer. Living with someone who smokes is estimated to increase the risk of lung cancer by up to 30% in people who don’t smoke.
- Exposure to asbestos – People who are exposed to asbestos are more likely to develop lung cancer or pleural mesothelioma. Although the use of asbestos in building materials has been banned across Australia since 2004, there is still asbestos in some older buildings and fences.
- Exposure to other elements – People who have been exposed to radioactive gas (radon), such as uranium miners, have an increased risk of lung cancer. Outdoor and indoor air pollution (e.g. exposure to household air pollution from gas, oil, or wood-burning cooking or heating) is another risk factor. Contact with the processing of arsenic, cadmium, steel and nickel, and exposure to diesel engine exhaust and welding fumes while working may also be risk factors. Working with materials containing crystalline silica (e.g. stone, sand, rock, bricks, tiles, concrete, artificial stone) can generate silica dust, which may cause a lung disease called silicosis when breathed in and is a risk factor for lung cancer. The use of engineered stone has been banned in Australia since July 2024.
Personal factors
- Older age – Lung cancer is diagnosed mostly in people aged over 60 years, although it can occur in younger people.
- Family history – You may be at a slightly higher risk if a family member has been diagnosed with lung cancer.
- Other conditions – Having another lung disease - lung fibrosis, chronic bronchitis, pulmonary tuberculosis, emphysema or COPD (chronic obstructive pulmonary disease) - or human immunodeficiency disease (HIV) may increase the risk of lung cancer.
Lung cancer symptoms
The main symptoms of lung cancer are:
- a new cough lasting more than three weeks, or a cough you've had for a long time that gets worse
- breathlessness or wheezing
- chest and/or shoulder pain
- a chest infection that is recurring or lasts more than three weeks
- coughing or spitting up blood.
Lung cancer may also cause other more general symptoms such as fatigue, weight loss, hoarse voice, difficulty swallowing, abdominal (belly) or joint pain, neck or face swelling, sweats and enlarged fingertips (finger clubbing).
Having any of these symptoms does not necessarily mean that you have lung cancer; they may be caused by other conditions or from other effects of smoking.
Sometimes, there are no symptoms and the cancer is found during routine tests for other conditions. If you have symptoms, see your doctor without delay.
Contact cancer support
When you call the Cancer Council support line on 13 11 20, you’ll talk to a cancer nurse and get the support you need.
It’s free, confidential, and available for anyone affected by cancer who has a question – those diagnosed as well as their family, friends, and carers.
Get support
Health professionals you will see
Your general practitioner (GP) will organise the first tests to assess your symptoms. If these tests do not rule out cancer, you will usually be referred to a respiratory physician, who will arrange further tests.
If lung cancer is diagnosed, the specialist will consider treatment options. Often these will be discussed with other health professionals at what is known as a multidisciplinary team (MDT) meeting.
During and after treatment you will see a range of health professionals, which may include a thoracic surgeon, medical oncologist, dietician and psychologist, who specialise in different aspects of your care.
Find support services in your area