Page last updated: January 2024
The information on this webpage was adapted from Understanding Skin Cancer - A guide for people with cancer, their families and friends (2024 edition). This webpage was last updated in January 2024.
Expert content reviewers:
This information was developed based on Australian clinical practice guidelines, and with the help of a range of health professionals and people affected by skin cancer:
- A/Prof Victoria Mar, Director, Victorian Melanoma Service, Alfred Hospital and Monash University, VIC
- Tracey Bilson, Consumer
- Raelene Buchan, Consumer
- Alison Button-Sloan, Consumer
- Dr Margaret Chua, Radiation Oncologist, and the Skin Radiation Oncology team, Peter MacCallum Cancer Centre, VIC
- Prof Anne Cust, Deputy Director, The Daffodil Centre, The University of Sydney and Cancer Council NSW Chair, National Skin Cancer Committee, Cancer Council, and faculty member, Melanoma Institute Australia
- A/Prof Paul Fishburn, Skin Cancer Doctor, Norwest Skin Cancer Centre, NSW and Faculty of Medicine, University of Queensland
- Danielle Goss, Melanoma Clinical Nurse Specialist, Amie St Clair Melanoma (part of Melanoma Institute Australia), Wagga Wagga, NSW
- Louise Pellerade, 13 11 20 Consultant, Cancer Council WA
- Dr Shireen Sidhu, Head of Dermatology, The Royal Adelaide Hospital, SA
- Dr Amelia Smit, Research Fellow – Melanoma and Skin Cancer, The Daffodil Centre, The University of Sydney and Cancer Council NSW
- Dr Tony Tonks, Plastic and Reconstructive Surgeon, Canberra Plastic Surgery, ACT
How do I spot a skin cancer?
Most skin cancers are self-detected. If you know your risk factors and what changes to watch for, you'll be more likely to find a skin cancer early.
Skin cancers don’t all look the same, but there are some signs to look out for, including:
- a spot that looks and feels different from other spots on your skin
- a spot that has changed size, shape, colour or texture
- a spot that is tender or sore to touch
- a sore that doesn’t heal within a few weeks
- a sore that is itchy or bleeds.
Getting to know your skin will help you notice any new or changing spots. Make a time to regularly check your skin.
There is no set guideline on how often to check for skin cancer, but if you have had a skin cancer or are at greater risk of developing skin cancer, your doctor can tell you how often to check your skin.
How to check your skin
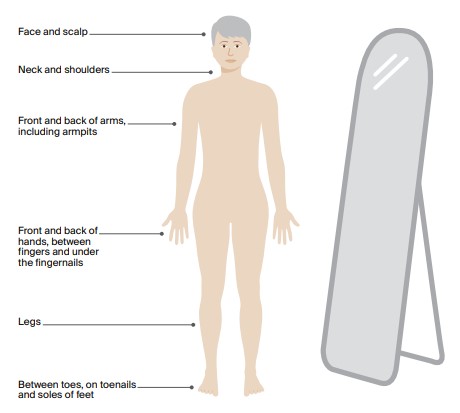
In a room with good light, undress completely and use a full-length mirror to check your whole body. To check areas that are difficult to see, use a handheld mirror or ask someone to help you.
If there any changes to your skin, if you notice something new, or you are worried about a spot you see, make an appointment with your doctor straightaway.
You will have a better outcome if the skin cancer is found and treated early.
Learn more
Which health professionals will I see?
You may see one or more of the following doctors to diagnose and treat skin cancer:
- General practitioner (GP) – many treat people with BCCs and SCCs. Treatment may include surgery, cryotherapy and/or topical treatments. You may be referred to a dermatologist, surgeon or radiation oncologist for larger areas.
- Dermatologist – a doctor who diagnoses, treats and manages skin conditions and skin cancer. They perform surgery, cryotherapy and prescribe topical treatments.
- Radiation or medical oncologist – a radiation oncologist treats some skin cancers by prescribing and overseeing a course of radiation therapy. A medical oncologist prescribes cancer drug therapies for some advanced skin cancers.
- Surgeon – some skin cancers are treated by specialised surgeons. These include surgical oncologists, who manage complex skin cancers, and plastic surgeons, who are trained in complex reconstructive techniques for more difficult to treat areas, such as the nose, lips, eyelids and ears.
Some GPs have extra training related to skin cancer. Before choosing a GP, you can ask what experience or qualifications they have with skin cancer.
You may see a GP at a general practice, medical centre or skin cancer clinic. Skin cancer clinics are run by GPs with an interest in skin cancer.
If there's a waiting list and a spot on your skin you are worried about, your GP can ask for an earlier appointment.
Question checklist
Asking your doctor questions will help you make an informed choice. You may want to include some of these questions in your own list:
Diagnosis
- What is this spot on my skin?
- Will I need a biopsy or excision?
- What is my biopsy result? Do I have skin cancer?
- What type of skin cancer is it?
- Did the biopsy or excision remove all the skin cancer?
- Are there clinical guidelines for this type of cancer?
Treatment
- What treatment will I have?
- Do I need further treatment or follow-up? If so, what treatment do you recommend?
- Do I need to see a dermatologist or surgeon?
- I’m thinking of getting a second opinion. Can you recommend anyone?
- How long will treatment take?
- If I don’t have the treatment, what should I expect?
- Are there any out-of-pocket expenses not covered by Medicare or my private health cover? Can the cost be reduced if I can’t afford it?
Side effects
- Will I have a lot of pain? What will be done about this?
- Can I work, drive and do my normal activities while having treatment?
- Will there be any scarring after the skin cancer has been removed?
- When will I get my results and who will tell me?
After treatment
- Is this skin cancer likely to come back?
- How often should I get my skin checked?
- Where can I go for follow-up skin checks?
- Will I need any further tests after treatment is finished?
- How can I prevent further skin cancers?
Can smartphone apps help detect skin cancer?
Some smartphone apps let you photograph your skin at regular intervals and compare the photos to check for changes. These apps may be a way to record any spot you are worried about or remind you to check your skin.
However, research shows apps cannot reliably detect skin cancer. If you notice a spot that causes you concern, make an appointment with your doctor straightaway.
Speak to a cancer nurse
Main tests
Physical examination
If you notice any changes to your skin, your doctor will look carefully at your skin and examine any spots you think are unusual. The doctor may use a handheld magnifying instrument called a dermoscope to examine the spots more closely.
They will also usually do a total body skin check to look at all your other moles and spots.
Skin biopsy
If your doctor feels they can diagnose the skin cancer by examining the spot, you may not need any further tests before having treatment.
However, it’s not always possible to tell the difference between a skin cancer and a non-cancerous skin spot just by looking at it.
If there is any doubt, the doctor may need to take a tissue sample (biopsy) to confirm the diagnosis. A biopsy is a quick and simple procedure that is usually done in the doctor’s room.
You will be given a local anaesthetic to numb the area, and then the doctor will either:
- completely cut out the spot and a small amount of healthy tissue around it to be tested (excision biopsy)
- take a small piece of tissue from the spot to be tested (punch or shave biopsy).
Stitches may be used to close a larger wound. After a biopsy, your doctor will give you instructions on how to look after the wound. The biopsy skin tissue is sent to a laboratory where a pathologist examines it under a microscope.
Your doctor will get the results in 1–2 weeks. If all the cancer and a margin of healthy tissue are removed during the biopsy, this may be the only treatment you need.
If the doctor has only taken a small piece from a larger spot, and this is found to be cancer, you will need to go back to have the rest of the cancerous spot removed.
Staging and prognosis
The stage of a cancer describes its size and whether it has spread. BCCs rarely need staging because they don’t often spread or have other high-risk features.
Only a very small number of SCCs require staging. This may be because of where the SCC is, its size or because it has spread.
Usually a biopsy is the only information a doctor needs to stage skin cancer. The doctor may also feel the lymph nodes near the skin cancer to check for swelling, as this may be a sign that the cancer has spread.
Prognosis means the expected outcome of a disease. Your treating doctor is the best person to talk to about your prognosis. Most BCCs and SCCs are successfully treated, especially when found early.
If you have any concerns or want to talk to someone, see your doctor or call 13 11 20.