Page last updated: March 2024
The information on this webpage was adapted from Understanding Secondary Bone Cancer - Information for people affected by cancer (2020 edition). This webpage was last updated in March 2024.
Expert content reviewers:
This information was developed with the help of a range of health professionals and people affected by secondary bone cancer:
- Dr Craig Lewis, Conjoint Associate Professor UNSW, Senior Staff Specialist, Department of Medical Oncology, Prince of Wales Hospital, NSW
- Dr Katherine Allsopp, Staff Specialist, Palliative Medicine, Westmead Hospital, NSW
- Michael Coulson, Consumer
- Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA
- David Phelps, Consumer
- Juliane Samara, Nurse Practitioner Specialist Palliative Care, Clare Holland House, Calvary Public Hospital Bruce, ACT
- A/Prof Robert Smee, Radiation Oncologist, Nelune Cancer Centre, Prince of Wales Hospital, NSW.
This page will help you understand more about secondary bone cancer - cancer that has spread to the bone from another part of the body.
After finding out that you have advanced cancer, you may feel a range of emotions including fear, anxiety, sadness, depression or anger. Your doctor, nurses, a social worker or counsellor can help you and your family find ways to cope with how you're feeling.
Call Cancer Council 13 11 20 for more information and support.
What is secondary bone cancer?
Bone cancer can develop as either a primary or secondary cancer. These two types are different:
- Primary bone cancer means the cancer starts in the bone.
- Secondary bone cancer means the cancer started in another part of the body but has now spread (metastasised) to the bone. It may also be called metastatic bone cancer, bone metastases or bone mets.
Secondary bone cancer keeps the name of the original cancer and is considered advanced, or stage 4, cancer because it has spread.
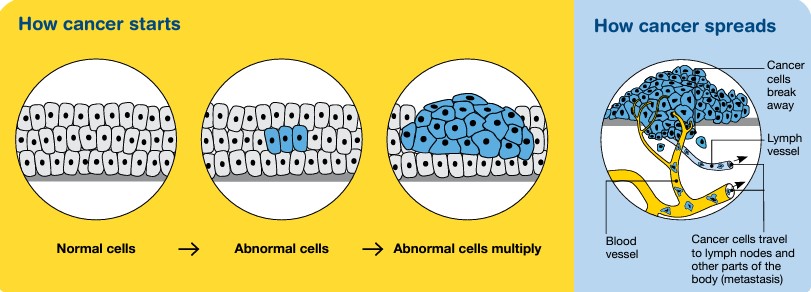
Cancer cells can spread from the original cancer, through the bloodstream or lymph vessels, to any of the bones in the body.
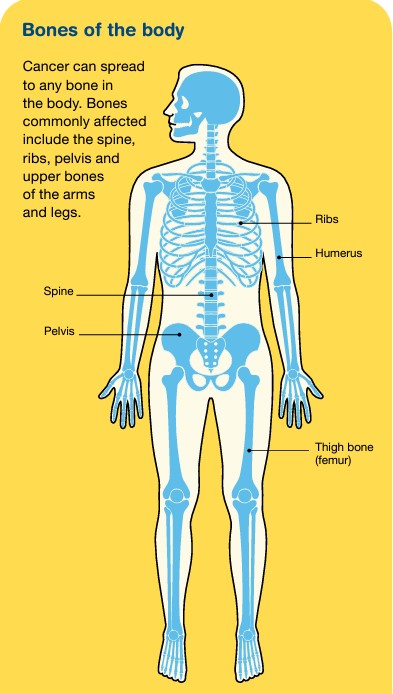
Bones commonly affected by secondary bone cancer include the:
- spine
- ribs
- pelvis
- upper bones of the arms (humerus) and legs (femur).
Any type of cancer can spread to the bone, but those most likely include:
- breast cancer
- kidney cancer
- lung cancer
- prostate cancer
- thyroid cancer
- melanoma (a type of blood cancer)
- myeloma.
How common is secondary bone cancer?
Secondary bone cancer is much more common than primary bone cancer in Australia and it is more common in adults than children. The bone is one of the most common sites cancer may spread to, along with the lymph nodes, liver, lungs and brain.
Secondary bone cancer is always caused by cancer cells spreading to the bone from a primary cancer. It is not fully understood why some people develop secondary bone cancer and others don’t.
About the bones
A typical healthy adult has over 200 bones, which:
- support and protect internal organs
- are attached to muscles to allow movement
- contain bone marrow, which produces and stores new blood cells
- store proteins, minerals and nutrients, such as calcium.
The bones are made up of different parts, including a hard outer layer (known as cortical or compact bone) and a spongy inner core (known as trabecular or cancellous bone), where bone marrow is found.
Cartilage is the tough material at the end of each bone that allows one bone to move against another. This meeting point is called a joint.
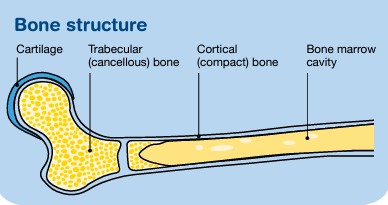
Bones have two types of cells – osteoblasts, which create new bone, and osteoclasts, which break down old bone. Normal bone is constantly going through a process called remodelling, in which old bone is broken down and replaced with new bone.
Types of secondary bone cancer
Secondary bone cancer is categorised as two main types:
- Osteolytic - where bone is broken down without new bone being made. In some cases, holes form in the bone, called lytic lesions. They can weaken the bone and increase the risk of breakage or other problems.
- Osteoblastic - where new bone is formed in some areas, but it grows abnormally. These areas are called osteoblastic lesions and they are very hard (dense) but they make the bone weak and deformed.
Most people with secondary bone cancer develop either osteolytic or osteoblastic changes, but some have both.
What are the symptoms?
The symptoms of secondary bone cancer are:
- Bone pain
- Fractures
- High calcium levels in the blood (hypercalcaemia)
- Pressure on the nerves in the spine (spinal cord compression)
- Low levels of blood cells
Bone pain is often the first and most common symptom. The pain may be a dull, persistent ache, can get worse with movement, and is often worse at night.
Cancer cells can weaken the bones and cause them to break more easily, often with little or no force (known as a pathological fracture). As the bone breaks down, calcium is released into the bloodstream. When calcium builds up in the blood, it may cause severe tiredness (fatigue), a feeling of sickness (nausea), vomiting, thirst, constipation or confusion.
Abnormal bone growth or fractures can press on the nerves in the spine. This may cause back pain, muscle and limb weakness, tingling or numbness of the limbs, difficulty walking, or loss of bowel or bladder control.
Secondary bone cancer can affect the bone marrow, particularly if there is a large amount of spread to the bones. The bone marrow makes blood cells, so the cancer can lead to low levels of blood cells.
Symptoms depend on the type of blood cell affected but can include feeling tired and breathless, having an increased risk of infections, or bruising and bleeding more easily.
Finding support
When you call the Cancer Council support line on 13 11 20, you’ll talk to a cancer nurse and get the support you need.
It’s free, confidential, and available for anyone affected by cancer who has a question – those diagnosed as well as their family, friends, and carers.
Contact cancer support
Diagnosis
Secondary bone cancer is sometimes found at the same time as the primary cancer. It can also be found months or years after the primary cancer has been treated.
Sometimes, secondary bone cancer is diagnosed before the primary cancer is found, and in some cases, the primary cancer cannot be found.
When tests can’t find where the cancer started, this is known as cancer of unknown primary (CUP). CUP can occur in other parts of the body as well as in the bone.
If your doctor is concerned the cancer has spread to the bones, you may have some of the following tests:
- blood tests – including a full blood count and a check of your calcium levels.
- bone x-ray – a scan of the chest and bones to show bone damage, fractures or creation of new bone.
- bone scan – a small amount of radioactive dye is injected into a vein and collects in the bone. Any abnormal changes are found by a special camera and computer.
- CT or MRI scans – a special computer is used to scan and create cross-sectional pictures to highlight any bone abnormality.
- PET–CT scan – a small amount of radioactive glucose solution is injected to highlight any cancerous areas.
- bone biopsy – removes some cells and tissues from the outer part of the affected bone for examination under a microscope. The biopsy may be done as a core biopsy or a surgical biopsy.
Prognosis
Prognosis means the expected outcome of a disease. You may want to discuss your prognosis and treatment options with your doctor.
Factors that affect prognosis include:
- whether the cancer has spread to other parts of your body
- how quickly it is growing
- how it responds to treatment.
It is not possible for anyone to predict the exact course of the disease, but your doctor can provide you with general information on the expected outcomes of people in a similar situation to you.
Secondary bone cancer can’t be cured, but treatment can reduce symptoms and improve quality of life. In some cases, treatment can keep secondary bone cancer under control for many years.
Understanding Secondary Bone Cancer
Download our Understanding Secondary Bone Cancer fact sheet to learn more.
Download now