Page last updated: March 2024
The information on this webpage was adapted from Understanding Melanoma - A guide for people with cancer, their families and friends (2021 edition). This webpage was last updated in March 2024.
Expert content reviewers:
This information is based on Australian clinical practice guidelines, and was developed with the help of a range of health professionals and people affected by melanoma:
- A/Prof Robyn Saw, Surgical Oncologist, Melanoma Institute Australia, The University of Sydney and Royal Prince Alfred Hospital, NSW
- Craig Brewer, Consumer
- Prof Bryan Burmeister, Radiation Oncologist, GenesisCare Fraser Coast and Hervey Bay Hospital, QLD
- Tamara Dawson, Consumer, Melanoma & Skin Cancer Advocacy Network
- Prof Georgina Long, Co-Medical Director, Melanoma Institute Australia, and Chair, Melanoma Medical Oncology and Translational Research, Melanoma Institute Australia, The University of Sydney and Royal North Shore Hospital, NSW
- A/Prof Alexander Menzies, Medical Oncologist, Melanoma Institute Australia, The University of Sydney, Royal North Shore and Mater Hospitals, NSW
- Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA
- Paige Preston, Chair, Cancer Council’s National Skin Cancer Committee, Cancer Council Australia
- Prof H Peter Soyer, Chair in Dermatology and Director, Dermatology Research Centre, The University of Queensland Diamantina Institute, and Director, Dermatology Department, Princess Alexandra Hospital, QLD
- Julie Teraci, Clinical Nurse Consultant and Coordinator, WA Kirkbride Melanoma Advisory Service, WA
This page includes information on melanoma, a type of skin cancer. Other types of skin cancer include basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), which are often called non-melanoma skin cancers.
Many people feel shocked and upset when told they have melanoma. If you have any questions or concerns, contact cancer support by calling Cancer Council 13 11 20.
What is melanoma?
Melanoma is a type of skin cancer. It develops in skin cells called melanocytes and usually occurs on parts of the body that have been overexposed to the sun.
Rare melanomas can start inside the eye or in a part of the skin or body that has never been exposed to the sun, such as mucous membrane (e.g. sinuses, digestive tract, genitals), soles of the feet or palms of the hand, and under the nails.
Although it is one of the less common types of skin cancer, melanoma is considered the most serious because it is more likely to spread to other parts of the body, especially if not detected early.
Your guide to best cancer care
A lot can happen in a hurry when you’re diagnosed with cancer. The guide to best cancer care for melanoma can help you make sense of what should happen.
It will help you with what questions to ask your health professionals to make sure you receive the best care at every step.
Read the guide
About the skin
The skin is the largest organ of the body. It acts as a barrier to protect the body from injury, control body temperature and prevent loss of body fluids.
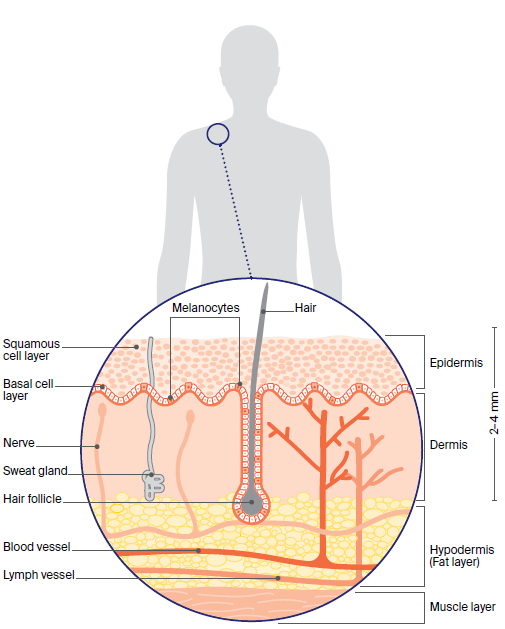
The two main layers of the skin are the epidermis and the dermis. Below these is a layer of fatty tissue known as the hypodermis.
Epidermis
The epidermis is the top, outer layer of the skin. It is made up of several sublayers that work together to continually rebuild the surface of the skin. The main sublayers are the basal cell layer and the squamous cell layer.
Basal cell layer
This is the lowest layer of the epidermis. It contains basal cells and cells called melanocytes. The melanocyte cells produce a dark pigment called melanin, which gives skin its colour.
When skin is exposed to ultraviolet (UV) radiation, melanocytes make melanin to try to protect the skin from getting burnt. This is what causes skin to tan.
When melanocytes cluster together they form non-cancerous spots on the skin called moles or naevi.
Squamous cell layer
This sits above the basal cell layer. Basal cells that have matured move up into the squamous cell layer. Here they are known as squamous cells or keratinocyte cells.
Squamous cells are the main type of cell found in the epidermis.
Dermis
The Dermis is the layer of the skin that sits below the epidermis. The dermis is made up of fibrous tissue and contains the roots of hairs (follicles), sweat glands, blood vessels, lymph vessels, and nerves.
How common is melanoma?
Australia and New Zealand have the highest rates of melanoma in the world. Melanoma is the second most common cancer in men and the third most common cancer in women (excluding non-melanoma skin cancers).
Every year in Australia, about 17,800 people are diagnosed with melanoma that has spread to the dermis (known as invasive melanoma).
About 27,500 people are diagnosed each year with melanoma that is confined to the epidermis (melanoma in situ) according to the Australian Institute of Health and Welfare.
Learn more
Types of melanoma
The major subtypes of melanoma of the skin (cutaneous melanoma) are:
- Superficial spreading melanoma
- Nodular melanoma
- Lentigo maligna melanoma
- Acral lentiginous melanoma
- Desmoplastic melanoma
Superficial spreading melanoma
This makes up 55-60% of melanomas, and is the most common type of melanoma in people under 40 (but can occur at any age). It can start as a new brown or black spot that grows on the skin, or as an existing spot, freckle or mole that changes size, colour or shape.
It can develop on any part of the body but especially the trunk, and often grows slowly. It becomes more dangerous when it invades the lower layer of the skin (dermis).
Nodular melanoma
This type is 10-15% of melanomas, and is most commonly found in people over 65. It usually appears as a round, raised lump on the surface of the skin that is pink, red, brown or black and feels firm to touch. It may develop a crusty surface that bleeds easily.
It is usually found on sun-damaged skin on the head and neck. It is a fast-growing and aggressive form of melanoma, spreading quickly into the lower layer of the skin (dermis).
Lentigo maligna melanoma
This makes up 10-15% of melanomas, and most people with this type of melanoma are over 40. It begins as a large coloured spot (lentigo maligna). It is mostly found on sun-damaged skin on the face, ears, neck or head.
It may grow slowly and superficially over many years before it penetrates more deeply into the skin.
Acral lentiginous melanoma
This is a rare type of melanoma (only 1-2% of melanomas) that mostly affects people over 40. It commonly appears as a colourless or lightly pigmented area, which can be mistaken for a stain or bruise. In the nails, it most often presents as a long streak of pigment.
It is most commonly found on the skin on the soles of the feet or palms of the hands, or under the fingernails or toenails. It tends to grow slowly before becoming invasive.
Desmoplastic melanoma
This is another rare type of melanoma (1-2% of melanomas) that mostly affects people over 60. It starts as a firm, growing lump, often the same colour as your skin. It may be mistaken for a scar and can be difficult to diagnose.
It is mostly found on sun-damaged skin on the head or neck. It tends to be slower to spread than other types of melanoma but is often diagnosed later.
Melanoma risk factors
The main cause of all types of skin cancer is overexposure to ultraviolet (UV) radiation, which most often comes from the sun, but it can also come from artificial sources such as solariums (also known as tanning beds or sun lamps).
Anyone can develop melanoma. However, the risk is higher in people who have:
- unprotected exposure to UV radiation, particularly a pattern of short, intense periods of sun exposure and sunburn, such as on weekends and holidays
- lots of moles (naevi) – more than 10 moles above the elbow on the arms and more than 50 on the body
- lots of moles with an irregular shape and uneven colour (dysplastic naevi)
- pale, fair or freckled skin, especially if it burns easily and doesn’t tan
- light-coloured eyes (blue or green), and fair or red hair
- a previous melanoma or other type of skin cancer
- a strong family history of melanoma
- a weakened immune system from using immunosuppressive medicines for a long time.
Visit SunSmart to learn about protecting your skin.
Family history of melanoma
Sometimes melanoma runs in families. Often, this is because family members have a similar skin type or a similar pattern of sun exposure in childhood.
Only 1–2% of melanomas in Australia involve an inherited faulty gene. Some of these genes have been identified.
When two or more close relatives have been diagnosed with melanoma, especially if the person has been diagnosed with more than one melanoma on different areas of the skin and/or diagnosed with melanoma before the age of 40, then they may have an inherited faulty gene.
People with a strong family history of melanoma should protect and monitor their skin themselves, and have a professional skin check by a doctor every year from their early 20s. New moles after this age should be investigated.
Learn more
Symptoms of melanoma
Melanoma can vary greatly in the way it looks. In people who have lots of moles, melanoma usually stands out and looks different from the other moles. The first sign is often a new spot or a change in an existing mole:
- size – the spot may appear or begin to grow larger
- colour – the spot may become blotchy with different depths and shades of colour (brown, black, blue, red, white, light grey, pink or skin-coloured)
- shape or border – the spot may increase in height, become scaly, have an irregular shape (scalloped or notched) or lack symmetry (the halves look different)
- itching or bleeding – the mole may itch or bleed very easily
- elevation – the spot may start as a raised nodule or develop a raised area, which is often reddish or reddish brown.
Checking your skin
New moles mostly appear during childhood and through to the 30s and 40s, as well as during pregnancy. However, adults of any age can have new or changing spots.
It is important to get to know your skin and check it regularly. In a room with good light, fully undress and use a full-length mirror to check your whole body.
For areas that are hard to see, use a handheld mirror or ask someone to help. Look for spots that are new, different from other spots, or raised, firm and growing.
Even if your doctor has said a spot is benign in the past, check for any changes in shape, size or colour. If you notice a new or changing spot, ask your doctor to examine it.
Learn more
Health professionals you'll see
You will probably start by seeing your general practitioner (GP). Some people choose to go to skin cancer clinics, which are often operated by GPs with an interest in skin cancer.
If a GP diagnoses or suspects melanoma, they will usually refer you to a specialist, such as a dermatologist or surgeon, who will arrange further tests and consider treatment options.
These options may be discussed with other health professionals, which may include a medical oncologist, reconstructive surgeon, cancer nurse coordinator and psychologist, at what is called a multidisciplinary team (MDT) meeting.
During and after treatment, you may also see a range of health professionals who specialise in different aspects of your care, especially if you have a melanoma with a Breslow thickness greater than 1 mm, or if the melanoma has spread.