What is appendix cancer?
Appendix cancer occurs when cells in the appendix become abnormal, and keep growing and form a mass or lump called a tumour.
The type of cancer is defined by the particular cells that are affected and can be benign (non-cancerous) or malignant (cancerous). Malignant tumours have the potential to spread to other parts of the body through the blood stream or lymph vessels and form another tumour at a new site. This new tumour is known as secondary cancer or metastasis.
The most common types of appendix cancer include:
- Mucinous adenocarcinoma – these start in epithelial cells that line the inside of the appendix. They can produce mucin (a jelly-like substance) and spread to other parts of the body, including the peritoneum, which is a sheet of tissue that lines and protects organs in the abdomen.
- Neuroendocrine tumours (NETs) – these form in neuroendocrine cells inside the appendix. The neuroendocrine system is a network of glands and nerve cells that make hormones and release them into the bloodstream to help control normal body functions. Appendiceal NETs are often found at the tip of the appendix.
- Goblet cell carcinoma (GCC) – these have features of both a NET and adenocarcinoma but behave more like an adenocarcinoma, which can be more aggressive.
- Colonic-type adenocarcinoma – these may behave like colon (large bowel) cancer and are often found at the base of the appendix.
What is PMP?
Pseudomyxoma peritonei (PMP) is a rare tumour that grows slowly and causes a build-up of mucin (a jelly-like substance) in the abdomen and pelvis, giving rise to the name 'jelly belly'. Several other diseases may also be associated with 'jelly belly' including mucinous adenocarcinoma, or may resemble features of PMP including mucinous tumours in the bowel.
PMP often starts in the appendix but can also start in other organs such as the large bowel and ovary. While it doesn’t spread to other parts of the body, PMP can put pressure on important organs as it continues to grow and this may cause problems.
About the appendix
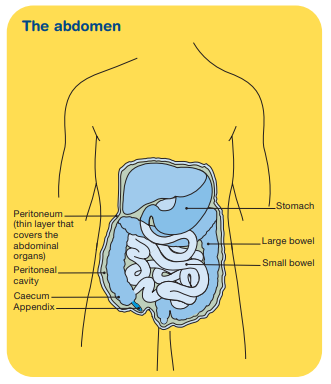
The appendix is a small tube that usually sits on the lower right side of the abdomen. It hangs off the end of the caecum, which is a pouch at the start of the large bowel. The appendix does not have a clear function, but is thought to store gut bacteria and may play a role in the immune system to help prevent disease.
How common are appendix cancer and PMP?
Appendix cancer is rare with 0.12 cases per 1,000,000 people each year being reported for primary malignancies (cancer that first develops in the appendix). The most common types are seen in middle-aged people, with 40 to 60 years being the typical age at diagnosis.
There is an almost equal risk for males and females for mucinous adenocarcinoma and GCC. Colonic-type adenocarcinoma is diagnosed slightly more often in men and appendiceal NETs are diagnosed more often in women.
PMP is also rare with about 1 or 2 cases per 1,000,000 people each year. It is more likely to be diagnosed in people aged 40 years or over. Women may be diagnosed slightly more often and at an earlier stage than men, after a mass or lump is found in their ovary.
Learn more about rare cancer
Symptoms
The causes of appendix cancer and PMP are not known. There are no clear risk factors and neither appear to run in families. Increasing age, however, can increase the risk of appendix cancer.
Appendix cancer may not cause symptoms in its early stages. However, some people may experience symptoms such as:
- appendicitis (lower right abdominal pain)
- gradual increase in waist size
- build-up of fluid in the abdomen
- bloating
- changes in bowel habits
- hernia
- ovarian mass or lump.
PMP is also difficult to detect, and symptoms may take a while to develop. Symptoms that some people may experience include:
- abdominal or pelvic pain
- gradual increase in waist size
- bloating
- changes in bowel habits
- hernia
- loss of appetite.
Diagnosis
Appendix cancer is often found during abdominal surgery for a different condition or after an appendectomy (surgical removal of the appendix) for a suspected case of appendicitis. Similarly, PMP is often discovered when investigating a different condition.
If your doctor thinks that you may have appendix cancer or PMP, they will perform a physical examination and carry out certain tests. If the results suggest that you may have appendix cancer or PMP, your doctor will refer you to a specialist who will carry out more tests.
Further tests
Further tests a specialist may carry out include:
- Blood tests – including a full blood count to measure your white blood cells, red blood cells, platelets and tumour markers (chemicals produced by cancer cells).
- CT (computerised tomography) or MRI (magnetic resonance imaging) scans – special painless machines are used to scan and create pictures of the inside of your body. Before the scan you may have an injection of dye into one of your veins, which makes the pictures clearer.
- Ultrasound scan – soundwaves are used to create pictures of the inside of your body.
- Diagnostic laparoscopy – a thin tube with a camera on the end (laparoscope) is inserted under sedation into the abdomen to view inside the cavity.
- Biopsy – removal of some tissue from the affected area for examination under a microscope.
Finding a specialist
Rare Cancers Australia have a knowledge-base directory of health professionals and cancer services across Australia. Pseudomyxoma Survivor have a directory of PMP surgeons and specialists in Australia.
Treatment
You will be cared for by a multi-disciplinary team of health professionals during your treatment, which may include a medical oncologist, surgeon, dietitian and physiotherapist, among others. Discussion with your doctor will help you decide on the best treatment for your cancer depending on:
- the type of cancer you have
- where it is in your body
- whether or not the cancer has spread (stage of disease)
- your age, fitness and general health
- your preferences.
The main treatments for appendix cancer and PMP are surgery and chemotherapy. These can be given alone or in combination and are an effective treatment, with a little over 60% of patients receiving both cytoreductive surgery and HIPEC surviving beyond 10 years.
PMP may not be treated straight away if the tumour is small and growing slowly. In this case it will be observed and monitored regularly, an approach known as active surveillance.
Complementary therapies are designed to be used alongside conventional medical treatments (such as surgery) and can increase your sense of control, decrease stress and anxiety, manage fatigue and improve your mood.
Surgery
Surgery is the main treatment for appendix cancer, especially for people with early-stage disease who are otherwise in good health. The type of operation depends on the location and stage of the tumour.
PMP is usually treated with surgery, either as cytoreductive surgery followed by chemotherapy (HIPEC) when aiming to cure PMP, or if the cancer cannot be treated effectively, debulking surgery may be used instead to remove as much of the tumour as possible to reduce symptoms. Debulking surgery may be done again if the tumour grows back.
Types of surgery include:
- Appendectomy – surgery to remove the appendix. Often used for early stage appendiceal NETs.
- Hemicolectomy – surgery to remove a small part of the large bowel next to the appendix. Surrounding lymph nodes and blood vessels may also be removed. Often used for appendiceal NETs at risk of spreading or appendix cancers that are not neuroendocrine.
- Cytoreductive surgery (CRS or peritonectomy) – surgery to remove all visible tumour from the abdominal cavity. Part of the bowel and other organs including gallbladder, spleen, stomach and kidney may also be removed. In females the uterus, ovaries and fallopian tubes may be removed. In males the seminal vesicles may be severed. Often used for late-stage appendix cancer and PMP. Chemotherapy may be used after the surgery.
General side effects of surgery include bleeding, damage to nearby tissue and organs (including nerves), drug reactions, pain, infection after surgery, blood clots, weak muscles (atrophy) and lymphoedema.
Side effects of CRS or peritonectomy may include bowel leaks and slow return to normal bowel function, dehydration and loss of fertility.
If part of the bowel is removed during surgery, the surgeon will usually join it back together. This join is called an anastomosis. If this isn’t possible, you may need a stoma, where the end of the intestine is brought through an opening made in your abdomen to allow faeces to be removed from the body and collected in a bag. The stoma may be temporary or permanent. For more information, visit the Australian Association of Stomal Therapy Nurses.
Chemotherapy
Chemotherapy is the use of drugs to kill or slow the growth of cancer cells. There are different types of chemotherapy used to treat appendix cancer and PMP:
- Local chemotherapy – where the chemotherapy drugs are delivered directly to the cancer. When placed directly in the abdomen it is called intraperitoneal chemotherapy.
- Systemic chemotherapy – where the chemotherapy drugs enter the bloodstream and travel throughout the body to target rapidly dividing cancer cells in the organs and tissues. This type of chemotherapy is given through a drip into a vein or as a tablet that is swallowed.
Types of intraperitoneal chemotherapy include:
- HIPEC (heated intraperitoneal chemotherapy) – the chemotherapy drug is heated to around 40°C (body temperature is about 37°C) to increase its effectiveness and placed directly in the abdomen to kill any tumour cells that remain after surgery or help control ascites (build-up of fluid). It is typically removed after 30–90 minutes.
- EPIC (early post-operative intraperitoneal chemotherapy) – the chemotherapy drug is delivered to the abdomen the day after surgery using an access port (small plastic device) and continued for several days. It is usually used after HIPEC when able to be tolerated.
Side effects may include fatigue, loss of appetite, nausea, bowel issues such as constipation or diarrhoea, hair loss, mouth sores, skin and nail problems, increased chance of infections and loss of fertility.
Radiation therapy
Radiation therapy uses high energy rays to destroy cancer cells. It may be used for appendix cancer when it has spread to other parts of the body, such as the bone. Radiation therapy can shrink the cancer and relieve symptoms.
A course of radiation therapy needs careful planning. It does not hurt and is usually given in small doses over a period of time to minimise side effects.
Side effects may include fatigue, loss of appetite, nausea, bowel issues such as diarrhoea, abdominal cramps and excess wind, bladder issues, hair loss, dry mouth, skin problems, lymphoedema and loss of fertility.
Treatment and fertility
One issue that is important to discuss before you undergo treatment is fertility, particularly if you want to have children in the future. This is especially the case if during your abdominal or pelvic surgery your seminal vesicles are severed (in males) or your uterus, ovaries and/or fallopian tubes are removed (in females).
It can help to talk things through with a counsellor, psychologist, friend or family member. You can also speak with our compassionate and trusted cancer nurses by calling 13 11 20.
Learn more
Life after treatment
Once your treatment has finished, you will have regular check-ups to confirm that the cancer hasn’t come back. Ongoing surveillance for appendix cancer and PMP involves a schedule of ongoing scans and physical examinations. Maintaining a healthy body weight, eating well and being physically active are all important.
For some people appendix cancer and PMP do come back after treatment, which is known as a recurrence. This is most likely to happen within the first five years after treatment. If the cancer does come back, treatment will depend on where the cancer has returned to in your body and may include a mix of surgery, chemotherapy and radiation therapy.
In some cases of advanced cancer, treatment will focus on managing any symptoms, such as pain, loss of appetite and improving your quality of life, without trying to cure the disease. This is called palliative treatment.
Question checklist
Asking your doctor questions will help you make an informed choice about your treatment and care. You may want to include some of the questions below in your own list:
- How far has the cancer spread? What stage of cancer do I have?
- Have you treated this type of cancer before?
- What are the treatment options for me? What do you recommend and why?
- How will you consult with other specialists for my treatment?
- How long will treatment take?
- Is it possible to have surgery to try to cure my cancer?
- If I can have surgery, which type will I need and why?
- Do you use HIPEC only during surgery, or do you use EPIC afterwards for several days?
- What type of rehabilitation will I need after my surgery? How long will recovery take?
- What are the possible risks and side effects of my treatment? How will these be managed?
- Is this treatment covered by Medicare/private insurance? Will there be extra expenses?
- Are there any complementary therapies that might help me?
- What are the possible benefits and risks to joining a clinical trial? What is being tested and why? How many people will be involved in this trial?
Understanding Appendix Cancer and PMP
Download our Understanding Appendix Cancer and Pseudomyxoma Peritonei (PMP) fact sheet to learn more
Download now
Expert content reviewers:
John Henriksen, Consumer; Prof David Morris, Surgical Oncologist, St George Hospital, Sydney, NSW; Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA.
Page last updated:
The information on this webpage was adapted from Understanding Appendix Cancer and Pseudomyxoma Peritonei (PMP) - A guide for people affected by cancer (2021 edition). This webpage was last updated in September 2021.