A stoma is a surgically created opening in the abdomen that allows bowel movements (faeces, stools or poo) to leave the body. The end of the bowel is brought out through the opening and stitched onto the skin. Some people need a stoma after bowel surgery, which may be temporary or permanent.
Your guide to best cancer care
A lot can happen in a hurry when you’re diagnosed with cancer. The guide to best cancer care for bowel cancer can help you make sense of what should happen. It will help you with what questions to ask your health professionals to make sure you receive the best care at every step.
Read the guide
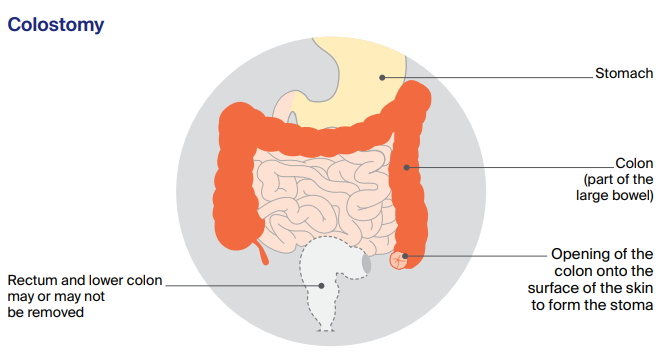
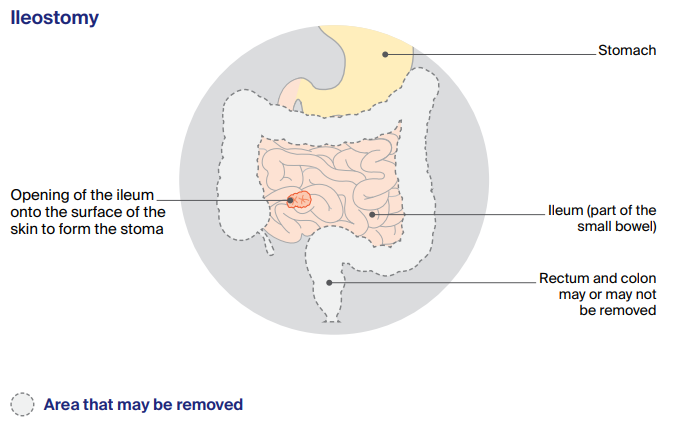
Types of stoma
The two types of stoma are a colostomy (made from the colon in the large bowel) and an ileostomy (made from the ileum in the small bowel).
A temporary stoma is only needed until the newly joined bowel has healed. In this situation, a loop stoma is often used, whereby a loop of the bowel is brought out, and then cut and stitched to the skin, creating two openings. You will have another operation, usually after 3 to 12 months, to close the stoma and rejoin the bowel. This is called a stoma reversal.
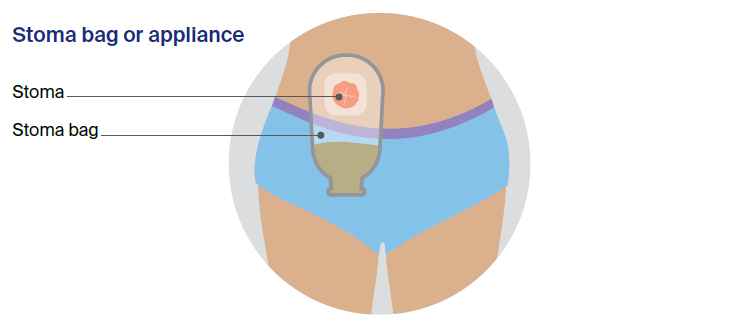
About 1 in 10 people with rectal cancer need a permanent stoma. Like the inside of the mouth, a stoma is soft, moist, and red or pink in colour. It may be level with the surrounding skin or slightly raised. The stoma itself doesn’t have any feeling, but the skin around it does. Stomas vary in size and can change shape during the weeks after surgery.
How the stoma works
When the bowel moves, wind and waste matter (faeces, stools or poo) come out through the stoma. You cannot control when this happens, so a small disposable bag is worn on the outside of the body to collect the waste. This is called a stoma bag or an appliance.
Stoma bags have adhesive on the back, so they stick firmly to the skin and provide a leak-proof, odour-proof system. A filter lets out any wind (but not the odour), which should stop the wind inflating the bag. The bag usually can’t be seen under clothing.
Some people don’t like to wear stoma bags. If you have a colostomy in your descending colon, you may be able to learn how to give yourself a type of enema (colostomy irrigation) to remove the waste every day or two. Talk to your doctor and stomal therapy nurse about this option.
Using a stoma
Attaching the bag
A stomal therapy nurse will help you choose an appliance that suits your body shape and the stoma, and will explain how to attach it securely.
Emptying the bag
Stoma bags can be drainable (able to be emptied) or closed (thrown out after each bowel movement). With a colostomy, the bag may be drainable or closed, depending on the consistency of your waste matter. With an ileostomy, you wear a drainable bag.
A drainable bag has to be emptied in the toilet when it is about one-third full. A closed bag should be put in a rubbish bin, not flushed down the toilet. A colostomy bag may need to be emptied 1 to 3 times a day depending on how much large bowel was removed, while an ileostomy bag may need to be emptied 4 to 6 times a day because the waste is more watery.
How often you need to empty a stoma bag is also affected by what you eat and drink.
Living with a stoma
Having a stoma, even temporarily, is a big change in a person’s life and takes some getting used to. However, thousands of Australians have a stoma and most lead a relatively normal life.
The stoma may sometimes affect your travel plans, social life and sexual relationships, but these issues can be managed, especially with some planning. Unless your job or hobbies are particularly strenuous, you should still be able to participate in your usual activities.
How a stoma might look
You may worry about how you will look. Although the stoma bag may seem obvious to you, most people won’t notice anything is different unless you tell them. The stoma’s location may make some clothes less comfortable (e.g. tight waistbands or belts), but you will generally be able to continue wearing your normal clothes. You might consider buying underwear designed for people with a stoma.
How a stoma might affect your sex life
Many people with a stoma worry that it will affect their ability to give or receive sexual pleasure. For men, creating a stoma usually involves removing part or all of at least one organ in the pelvic area. This may affect the nerves controlling erections. For women, if the rectum is removed, there may be a different feeling in the vagina during intercourse. It may be uncomfortable, as the rectum no longer cushions the vagina.
How a stoma might affect what you can eat
For people with a stoma, some foods can build up and cause blockages. This means solids, fluids and gas can’t move through as they normally would. To help the stoma settle and to avoid blockages, you may need to change what you eat. Over time, most people find they can eat a normal healthy diet. A stoma blockage can be uncomfortable and cause a bloated feeling or nausea. If you experience symptoms of a blockage for more than two hours or you start vomiting, contact your nurse or hospital.
Stoma prolapse
This is when some of the bowel comes out through the stoma opening. Sometimes the prolapse will slide back in by itself, but it may pop in and out. Your stomal therapy nurse or surgeon can tell you how to look after the prolapsed stoma and adapt the stoma bag.
Ways to manage stoma blockages
If you have a stoma, you may need to change what you eat in the first few weeks to help the stoma settle. The amount of stoma output will vary depending on how much and when you eat.
Here are some tips to manage stoma blockages:
- Eat regular meals.
- Avoid eating a large amount of food at one time.
- Try to maintain a balanced diet so your body is well nourished.
- Aim to drink 8–10 glasses of fluid a day so you stay well hydrated.
- Cut food into small, bite-sized pieces, and chew slowly and thoroughly.
- If you have trouble eating a certain food, talk to a dietitian about alternatives.
- You may find cooked food easier to digest.
- Limit foods that are more likely to cause blockages. These include high-fibre foods, raw vegetables, fruit and vegetable skins, nuts, seeds, kernels (e.g. corn, popcorn) and sausage skins.
- Have small amounts of a new food. If it doesn’t irritate the stoma, try more next time.
- Massage your belly and the area around the stoma. Lie on your back and pull your knees up to your chest and roll from side to side.
Support
See a stomal therapy nurse
If there is a chance you could need a stoma, the surgeon will probably refer you to a stomal therapy nurse before surgery. Stomal therapy nurses are registered nurses with special training in stoma care, and are available at most major hospitals, district nursing agencies and in private practice.
A stomal therapy nurse can talk to you about the best position for the stoma, answer questions about your surgery and recovery, and give you information about adjusting to life with a stoma. For more details, visit the Australian Association of Stomal Therapy Nurses or call Cancer Council on 13 11 20.
Join a stoma association
With your consent, the stomal therapy nurse will sign you up to a stoma (or ostomy) association. For a small annual membership fee, you will be able to obtain free stoma appliances and products. Stoma associations also provide assistance and information to members and coordinate support groups for people of all ages. The Australian Council of Stoma Associations represents stoma associations across Australia.
Register for the Stoma Appliance Scheme
The Australian Government’s Stoma Appliance Scheme (SAS) provides free stoma supplies to people with a temporary or permanent stoma. To apply for the SAS, you must hold a Medicare card and belong to a stoma association.
Understanding Bowel Cancer
Download our Understanding Bowel Cancer booklet to learn more.
Download now
Expert content reviewers:
A/Prof David A Clark, Colorectal Surgeon, Royal Brisbane and Women’s Hospital, and The University of Queensland, QLD, and The University of Sydney, NSW; A/Prof Siddhartha Baxi, Radiation Oncologist and Medical Director, GenesisCare Gold Coast, QLD; Dr Hooi Ee, Specialist Gastroenterologist and Head, Department of Gastroenterology, Sir Charles Gairdner Hospital, WA; Annie Harvey, Consumer; A/Prof Louise Nott, Medical Oncologist, Icon Cancer Centre, Hobart, TAS; Caley Schnaid, Accredited Practising Dietitian, GenesisCare, St Leonards and Frenchs Forest, NSW; Chris Sibthorpe, 13 11 20 Consultant, Cancer Council Queensland; Dr Alina Stoita, Gastroenterologist and Hepatologist, St Vincent’s Hospital Sydney, NSW; Catherine Trevaskis, Gastrointestinal Cancer Specialist Nurse, Canberra Hospital, ACT; Richard Vallance, Consumer.
Page last updated:
The information on this webpage was adapted from Understanding Bowel Cancer - A guide for people with cancer, their families and friends (2021 edition). This webpage was last updated in June2021.