Page last updated: April 2024
The information on this webpage was adapted from Understanding Pancreatic Cancer - A guide for people with cancer, their families and friends (2024 edition). This webpage was last updated in April 2024.
Expert content reviewers:
This information was developed based on clinical practice guidelines, and with the help of a range of health professionals and people affected by cervical cancer:
- Prof Lorraine Chantrill, Honorary Clinical Professor, University of Wollongong, and Head of Department, Medical Oncology, Illawarra Shoalhaven Local Health District, NSW
- Karen Baker, Consumer
- Michelle Denham, 13 11 20 Consultant, Cancer Council WA
- Prof Anthony J Gill, Surgical Pathologist, Royal North Shore Hospital and The University of Sydney, NSW
- A/Prof Koroush Haghighi, Liver, Pancreas and Upper Gastrointestinal Surgeon, Prince of Wales and St Vincent’s Hospitals, NSW
- Dr Meredith Johnston, Radiation Oncologist, Liverpool and Campbelltown Hospitals, NSW
- Dr Brett Knowles, Hepato-Pancreato-Biliary and General Surgeon, Royal Melbourne Hospital, Peter MacCallum Cancer Centre, and St Vincent’s Hospital, VIC
- Rachael Mackie, Upper GI – Clinical Nurse Consultant, Peter MacCallum Cancer Centre, VIC
- Prof Jennifer Philip, Chair of Palliative Care, University of Melbourne, and Palliative Medicine Physician, St Vincent’s Hospital, Peter MacCallum Cancer Centre and Royal Melbourne Hospital, VIC
- Lucy Pollerd, Social Worker, Peter MacCallum Cancer Centre, VIC
- Rose Rocca, Senior Clinical Dietitian – Upper GI, Peter MacCallum Cancer Centre, VIC
- Stefanie Simnadis, Clinical Dietitian, St John of God Subiaco Hospital, WA
Pancreatic cancer is cancer that starts in any part of the pancreas. About 75% of pancreatic cancers are found in the head of the pancreas.
Pancreatic cancer can spread to nearby lymph nodes and to the lining of the abdomen (peritoneum). Cancer cells may also travel through the bloodstream to other parts of the body, such as the liver.
Anatomy of the pancreas
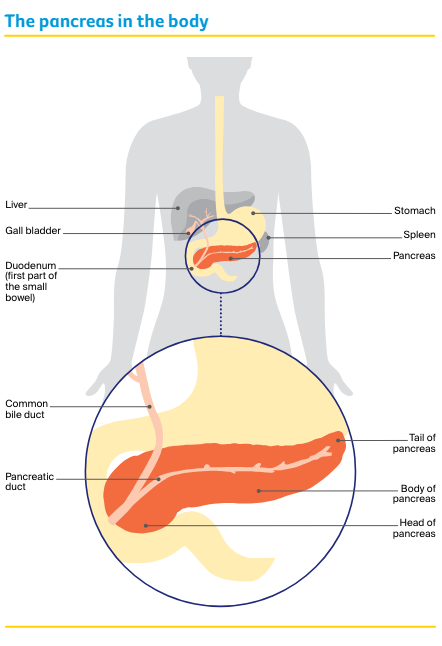
The pancreas is a long, flat gland about 13–15 cm long that lies between your stomach and spine. It is divided into three main parts:
- The head – the large rounded end
- The body – the middle part
- The tail – the narrow end that sits up next to your spleen.
A tube called the pancreatic duct connects the pancreas to the first part of the small bowel (duodenum). Another tube, called the common bile duct, joins with the pancreatic duct and connects the liver and gall bladder to the duodenum.
Function of the pancreas
The pancreas has two main jobs. It makes digestive juices (known as its exocrine function) and hormones (its endocrine function):
- Exocrine function – the pancreas is part of the digestive system, which helps the body digest food and turn it into energy. Exocrine cells make pancreatic enzymes, which are digestive juices. The pancreatic duct carries these juices from the pancreas into the duodenum, where they help to break down food. Most of the pancreas is made up of exocrine tissue.
- Endocrine function – the pancreas is also part of the endocrine system, a group of glands that makes the body’s hormones. Endocrine cells in the pancreas make hormones that control blood sugar levels, the amount of acid produced by the stomach, and how quickly food is absorbed.
Your guide to best cancer care
A lot can happen in a hurry when you’re diagnosed with cancer. The guide to best cancer care for pancreatic cancer can help you make sense of what should happen.
It will help you with what questions to ask your health professionals to make sure you receive the best care at every step.
Read the guide
Main types of pancreatic cancer
There are two main groups of pancreatic cancer:
- Exocrine tumours – these make up more than 95% of pancreatic cancers. The most common type is called adenocarcinoma, and it starts in the exocrine cells lining the pancreatic duct. Less common types include adenosquamous carcinoma, acinar cell carcinoma, squamous cell carcinoma and undifferentiated carcinoma.
- Pancreatic neuroendocrine tumours (NETs) – about 5% of cancers in the pancreas are pancreatic NETs. These start in the endocrine cells. Learn more about how pancreatic NETs are diagnosed and treated.
How common is pancreatic cancer?
About 4500 Australians are diagnosed with pancreatic cancer each year. More than 80% are over the age of 60. Pancreatic cancer was estimated to be the eighth most common cancer in Australia in 2023.
Pancreatic cancer affects men and women at about the same rate.
Learn more
Symptoms
Early-stage pancreatic cancer rarely causes obvious symptoms. Symptoms may not appear until the cancer is large enough to affect nearby organs or has spread.
The first symptom of pancreatic cancer is often jaundice. Signs of jaundice may include yellowish skin and eyes, dark urine, pale bowel motions and itchy skin.
Jaundice is caused by the build-up of bilirubin, a dark yellow-brown substance found in bile. Bilirubin can build up if pancreatic cancer blocks the common bile duct.
Other common symptoms of pancreatic cancer include:
- appetite loss
- nausea with or without vomiting
- unexplained weight loss
- pain in the upper abdomen, side or back, which may cause you to wake up at night
- changed bowel motions – including diarrhoea, severe constipation, or pale, oily, foul-smelling stools (poo) that are difficult to flush away
- bloating and passing wind and burping more than usual
- newly diagnosed type two diabetes
- fatigue.
These symptoms can also occur in many other conditions and do not necessarily mean that you have cancer. If you are worried or have ongoing symptoms, speak with your general practitioner (GP).
“I went to the doctor because I was itchy and had constant diarrhoea. My GP initially thought it was gallstones and sent me for routine tests. After the CT scan I went into hospital for a laparoscopy and then had a biopsy, which confirmed I had cancer.” Jan
Risk factors
The causes of pancreatic cancer are not known, but research has shown that people with certain risk factors are more likely to develop pancreatic cancer, including:
- smoking tobacco (smokers are about twice as likely to develop pancreatic cancer as non-smokers)
- obesity
- ageing
- long-term diabetes (but diabetes can also be caused by the pancreatic cancer)
- long-term pancreatitis (inflammation of the pancreas)
- certain types of cysts in the pancreatic duct known as intraductal papillary mucinous neoplasms (IPMNs) – these should be assessed by an appropriate specialist
- stomach infections caused by the Helicobacter pylori bacteria (which can also cause stomach ulcers)
- family history and inherited conditions
- workplace exposure to certain pesticides, dyes or chemicals.
Having risk factors does not mean you will definitely get cancer, but talk to your doctor if you are concerned. Some people with pancreatic cancer have no known risk factors.
Does pancreatic cancer run in families?
Most people diagnosed with pancreatic cancer do not have a family history of the disease.
Only about 5–10% of people who develop pancreatic cancer have inherited a faulty gene that increases the risk of developing pancreatic cancer.
You may have inherited a faulty gene linked to pancreatic cancer if:
- two or more of your close family members (such as a parent or sibling) have had pancreatic cancer
- there is a family history of a genetic condition, such as Peutz-Jeghers syndrome, the familial breast cancer genes (BRCA1 and BRCA2), familial atypical multiple mole melanoma (FAMMM) syndrome, Lynch syndrome and hereditary pancreatitis.
Genetic testing aims to find inherited faulty genes that may increase a person’s risk of developing some cancers. People with a strong family history of cancer can go to a family cancer clinic for genetic counselling.
Talk to your doctor, local family cancer clinic or call 13 11 20 cancer support for more information.
Learn more
Health professionals
Your GP will arrange the first tests to assess your symptoms. If these tests do not rule out cancer, you will usually be referred to a specialist, such as a gastroenterologist or surgeon, who will arrange further tests.
If pancreatic cancer is diagnosed, the specialist will consider treatment options. Often these will be discussed with other health professionals at what is known as a multidisciplinary team (MDT) meeting.
During and after treatment, you will see a range of health professionals who specialise in different aspects of your care, including a pancreatic or HPB (hepato-pancreatobiliary) surgeon, endocrinologist, radiologist and dietician, among others.
Where should I have treatment?
Treatment for pancreatic cancer is highly specialised. This is especially the case with surgery for early pancreatic cancer.
There is strong evidence that outcomes are better when people have their treatment in a specialist centre that sees a lot of people with pancreatic cancer.
These high-volume centres have multidisciplinary teams of health professionals experienced in treating pancreatic cancer.
Visiting one of these pancreatic cancer centres gives you access to a wide range of treatment options, including clinical trials, but it may mean you need to travel away from home to have the treatment.
Sometimes the multidisciplinary team from a specialist centre will be able to advise your local specialist. You may find that you can visit the specialist centre to confirm the diagnosis and work out a treatment plan and then have much of your treatment closer to your home.
To find a treatment centre that specialises in pancreatic cancer, talk to your GP. If you live in a rural or regional area and have to travel a long way for appointments or treatment, you may be able to get financial assistance.
Speak to your GP or the hospital social worker, or call 13 11 20 to find out more. You can also ask about accessing our Financial Counselling Program.
Question checklist
Asking your doctor questions will help you make an informed choice. You may want to include some of these questions in your own list:
Diagnosis
- What type of pancreatic cancer do I have?
- Has the cancer spread? If so, where has it spread? How fast is it growing?
- Are the latest tests and treatments for this cancer available in this hospital?
- Will a multidisciplinary team be involved in my care?
- Are there clinical guidelines for this type of cancer?
Treatment
- What treatment do you recommend? What is the aim of the treatment?
- Are there other treatment choices for me? If not, why not?
- If I don’t have the treatment, what should I expect?
- How long do I have to make a decision?
- I’m thinking of getting a second opinion. Can you recommend anyone?
- How long will treatment take? Will I have to stay in hospital?
- Are there any out-of-pocket expenses not covered by Medicare or my private health cover? Can the cost be reduced if I can’t afford it?
- How will we know if the treatment is working?
- Are there any clinical trials or research studies I could join?
- Do I need the support of a specialist palliative care service?
Side effects
- What are the risks and possible side effects of each treatment?
- Will I have a lot of pain? What will be done about this?
- Can I work, drive and do my normal activities while having treatment?
- Will the treatment affect my sex life and fertility?
- Should I change my diet or physical activity during or after treatment?
- Are there any complementary therapies that might help me?
After treatment for early pancreatic cancer
- How often will I need check-ups after treatment?
- If the cancer returns, how will I know? What treatments could I have?