Page last updated: January 2024
The information on this webpage was adapted from Understanding Cervical Cancer - A guide for people with cancer, their families and friends (2023 edition). This webpage was last updated in January 2024.
Expert content reviewers:
This information was developed based on international and Australian clinical practice guidelines, and with the help of a range of health professionals and people affected by cervical cancer:
- Prof Martin Oehler, Director of Gynaecological Oncology, Royal Adelaide Hospital, and Clinical Professor, University of Adelaide, SA
- Dawn Bedwell, 13 11 20 Consultant, Cancer Council QLD
- Gemma Busuttil, Radiation Therapist, Crown Princess Mary Cancer Centre, Westmead Hospital, NSW
- Dr Antonia Jones, Gynaecological Oncologist, The Royal Women’s Hospital and Mercy Hospital for Women, VIC
- Angela Keating, Senior Psychologist, Royal Hospital for Women, NSW
- Anne Mellon, Clinical Nurse Consultant – Gynaecological Oncology, Hunter New England Centre for Gynaecological Cancer, NSW
- Dr Inger Olesen, Medical Oncologist, Andrew Love Cancer Centre, Barwon Health, Geelong, VIC
- Dr Serena Sia, Radiation Oncologist, Fiona Stanley Hospital and King Edward Memorial Hospital, WA
- A/Prof Megan Smith, Co-lead, Cervical Cancer and HPV Stream, The Daffodil Centre, Cancer Council NSW and The University of Sydney, NSW
- Emily Stevens, Gynaecology Oncology Nurse Coordinator, Southern Adelaide Local Health Network, Flinders Medical Centre, SA
- Melissa Whalen, Consumer.
It is common to feel shocked and upset when told you have cervical cancer. We hope this page will help you, your family and friends understand how cervical cancer is diagnosed and treated.
If you or your family have any questions or concerns, call Cancer Council 13 11 20. We can send you more information and connect you with support services in your area.
What is cervical cancer?
Cervical cancer begins when abnormal cells in the lining of the cervix grow uncontrollably. Anyone with a cervix can get cervical cancer – women, transgender men and intersex people.
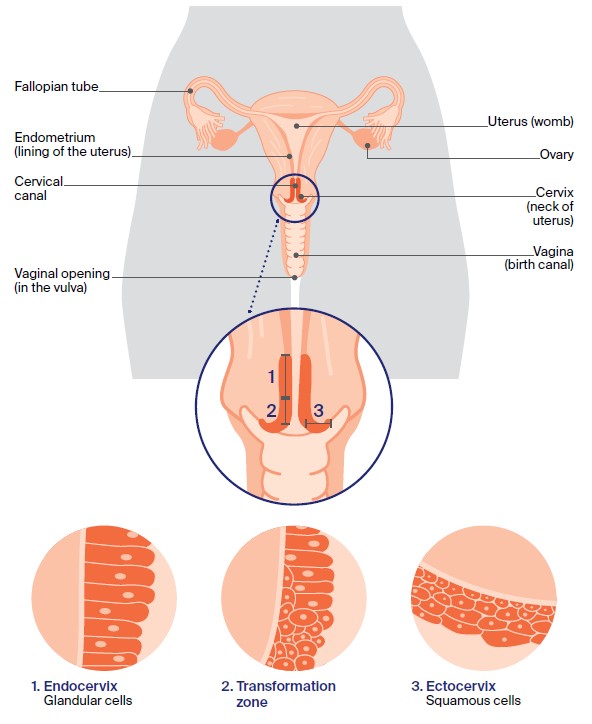
The cervix has an outer surface that opens into the vagina (ectocervix) and an inner surface that lines the cervical canal (endocervix). These surfaces are covered by two types of cells:
- Squamous cells – flat, thin cells that cover the outer surface of the cervix (ectocervix)
- Glandular cells – column-shaped cells that cover the inner surface of the cervix (cervical canal or endocervix).
The area where the squamous cells and glandular cells meet is known as the transformation zone. This is where most cervical cancers start.
The cancer may then spread to tissues around the cervix, such as the vagina, or to other parts of the body, such as the lymph nodes, lungs or liver.
About the cervix
The cervix is part of the female reproductive system, which also includes the ovaries, fallopian tubes, uterus (womb), vagina (birth canal) and vulva (external genitals). The cervix connects the uterus to the vagina and:
- produces fluid to help keep the vagina healthy
- opens to let menstrual blood pass from the uterus into the vagina
- produces mucus that helps sperm travel up the uterus and fallopian tubes to fertilise an egg that has been released from the ovary
- holds a developing baby in the uterus during pregnancy by remaining closed, then widens to let a baby be born through the vagina.
How common is cervical cancer?
Each year about 960 Australian women are diagnosed with cervical cancer. Cervical cancer is most commonly diagnosed in women over 30, but it can occur at any age.
In 2022, 206 Victorians were diagnosed with cervical cancer. Victorian Cancer Registry's most recent data shows that 5-year survival is 77% for the period 2017-2021.
Diagnoses of cervical cancer in Australia have reduced significantly since a national screening program was introduced in the 1990s.
The introduction of a national HPV vaccination program in 2007 and improvements to the screening program in 2017 are expected to further reduce rates of cervical cancer.
Learn more
Types
There are two main types of cervical cancer, which are named after the cells they start in.
Squamous cell carcinoma (SCC)
SCC is the most common type of cervical cancer (about 6 out of 10 cases), and starts in the squamous cells of the cervix.
Adenocarcinoma
Adenocarcinoma is a less common type of cervical cancer (about 3 out of 10 cases), and starts in the glandular cells of the cervix. It is more difficult to diagnose because it occurs higher up in the cervix and the abnormal glandular cells are harder to find.
Mixed carcinomas
A small number of cervical cancers (less than 1 in 20 cases) feature both squamous cells and glandular cells. These cancers are known as adenosquamous carcinomas or mixed carcinomas.
Other rarer types of cancer that can start in the cervix include small cell carcinoma, clear cell adenocarcinoma and cervical sarcoma.
Symptoms
Precancerous cervical cell changes usually have no symptoms. The only way to know if there are abnormal cells in the cervix that may develop into cancer is to have a cervical screening test. If symptoms occur, they usually include:
- vaginal bleeding between periods, after menopause, or during or after sexual intercourse
- pelvic pain
- pain during sexual intercourse
- a change to your usual vaginal discharge, e.g. there may be more discharge or it may have a strong or unusual smell or colour.
Any of these symptoms can happen for other reasons, but it is best to rule out cervical cancer. See your doctor if you are worried or the symptoms are ongoing.
This is important for anyone with a cervix, whether straight, lesbian, gay, bisexual, transgender or someone with an intersex variation, even if you are up to date with cervical screening tests.
If you’ve noticed any unexplained symptoms or want to get up-to-date with cancer screening, don't delay and visit a health professional.
Find a Health Professional
Precancerous cervical cell changes
Sometimes the squamous cells and glandular cells in the cervix start to change, and appear abnormal when iewed under a microscope.
These early cervical cell changes may be precancerous. This means there is an area of abnormal tissue (a lesion) that is not cancer, but may lead to cancer.
Some people with precancerous changes of the cervix will develop cervical cancer, so it is important to investigate any cervical cell changes.
How precancerous cell changes start
Precancerous cervical cell changes are caused by some types of the human papillomavirus (HPV). HPV and cervical cell changes don’t usually cause symptoms but can be found during a routine cervical screening test.
Finding and treating precancerous cervical cell changes will prevent them developing into cervical cancer.
Types of cervical cell changes
Abnormal squamous cells – these are called squamous intraepithelial lesions (SIL). They can be classified as either low grade (LSIL) or high grade (HSIL).
LSIL usually disappear without treatment, while HSIL can be precancerous. High-grade abnormalities have the potential to develop into early cervical cancer if they are not found and treated.
Abnormal glandular cells – high grade precancer in glandular cells is called adenocarcinoma in situ (AIS or ACIS). AIS is not cancer, but needs treatment to reduce the chance that it develops into adenocarcinoma.
What causes cervical cancer?
Almost all cases of cervical cancer are caused by an infection with the human papillomavirus (HPV), that affects the surface of different areas of the body, such as the cervix, vagina and skin.
There are more than 100 different types of HPV, including over 40 types that affect the genitals. Some types of HPV cause cancer, while others can cause common warts on the hands and feet.
Genital HPV is usually spread during close contact with genital skin during sexual activity. This includes penetrative sex as well as oral sex and other forms of sexuality (e.g. using sex toys).
Using condoms or dental dams offers some protection against HPV. About four out of five people will become infected with at least one type of genital HPV at some time in their lives.
Most people will not know they have HPV as it doesn’t cause symptoms. The virus is mostly cleared quickly by the immune system and no treatment is needed.
If the infection doesn’t go away, there’s an increased risk of developing changes in the cervix. These changes usually develop slowly over many years.
14 types of genital HPV are known to cause cervical cancer. Screening tests are used to detect most of these types of HPV or the precancerous cell changes caused by the virus.
There is also a vaccine that protects people from some types of HPV.
What is the cervical screening test?
Screening is organised testing to find precancer before it develops into cancer, as well as early cancer before symptoms appear.
The cervical screening test - which has replaced the Pap test - finds cancer-causing types of HPV in call samples taken from the cervix.
The National Cervical Screening Program recommends that women start cervical screening at age 25 and then have a test every five years up to the age of 70-74.
All people with a cervix need regular screening. There are two ways to collect cells for a cervical screening test, and in most cases you can choose the way you prefer:
Health provider collected
- During the test, a doctor or nurse gently inserts an instrument (called a speculum) into the vagina to widen the vaginal walls and get a clearer view of the cervix.
- They will then use a brush or spatula to remove some cells from the cervix. This can feel slightly uncomfortable, but usually takes only 1–2 minutes.
- The cell sample is then placed in a container of liquid and sent to a laboratory to check for HPV.
- If HPV is found, a specialist doctor called a pathologist will do an additional test on the sample to check for cell abnormalities. This is called liquid-based cytology (LBC).
Self-collected
- This is done in a private space (e.g. a bathroom) in a health clinic. A health care provider will give you a self-collection swab and explain how to collect your own cell sample.
- If you prefer, the provider can assist you to collect the sample without using a speculum. Self-collection is only available to people who do not have any signs or symptoms of cancer.
- Self-collected samples are not suitable for liquid-based cytology, so if HPV is detected, you may be asked to return to have a health provider collect a second sample or be referred for a colposcopy.
If the results show:
- a higher risk – your GP will refer you for a colposcopy
- an intermediate risk – you will be monitored for changes by having a follow-up test for HPV in 12 months
- a low risk – you will be due for your next cervical screening test in five years.
Other risk factors
Smoking and passive smoking
Chemicals in tobacco can damage the cells of the cervix, making it harder for the body to clear the HPV infection.
Using oral contraceptives (the pill) for a long time
Research has shown that taking the pill for five years or more increases the risk of developing cervical cancer in people with HPV. The reason for this is not clear.
However, the pill can also help protect against other types of cancer, such as uterine and ovarian cancers. Talk to your doctor if you are concerned.
Having a weakened immune system
The immune system helps rid the body of HPV. In some people, a weakened immune system can increase the risk of developing cervical cancer so more frequent cervical screening tests may be needed.
This includes people with the human immunodeficiency virus (HIV) and those who have had an organ transplant.
Health professionals
Your general practitioner (GP) will arrange the first tests to assess your symptoms. If these tests do not rule out cancer, you will usually be referred to a specialist, such as a gynaecologist or gynaecological oncologist, who will arrange further tests.
If cervical cancer is diagnosed, the specialist will consider treatment options. Often these will be discussed with other health professionals who specialise in different aspects of your care at what is known as a multidisciplinary team (MDT) meeting.
Get support
While we can provide information to answer some of your questions, we cannot give advice about the best treatment for you.
This needs to be discussed with your doctors. For support finding a health professional, call our cancer nurses on 13 11 20.
Contact cancer support