Page last updated: November 2025
The information on this webpage was adapted from Understanding Liver Cancer - A guide for people with cancer, their families and friends (2024 edition). This webpage was last updated in November 2025.
Expert content reviewers:
This information was developed based on international clinical practice guidelines and an Australian consensus statement. All updated content has been clinically reviewed by:
- A/Prof Simone Strasser, Head of Department and Hepatologist, AW Morrow Gastroenterology and Liver Centre, Royal Prince Alfred Hospital and The University of Sydney, NSW; and
- A/Prof Siddhartha Baxi, Radiation Oncologist and Medical Director, GenesisCare, Gold Coast, QLD.
This edition is based on the previous edition, which was reviewed by the following panel:
- A/Prof Simone Strasser (see above)
- A/Prof Siddhartha Baxi (see above)
- Prof Katherine Clark, Clinical Director of Palliative Care, NSLHD Supportive and Palliative Care Network, Northern Sydney Cancer Centre, Royal North Shore Hospital, NSW
- Anne Dowling, Hepatoma Clinical Nurse Consultant and Liver Transplant Coordinator, Austin Health, VIC
- A/Prof Koroush Haghighi, Liver, Pancreas and Upper Gastrointestinal Surgeon, Prince of Wales and St Vincent’s Hospitals, NSW
- Karen Hall, 13 11 20 Consultant, Cancer Council SA
- Dr Brett Knowles, Hepato-Pancreato-Biliary and General Surgeon, Royal Melbourne Hospital, Peter MacCallum Cancer Centre and St Vincent’s Hospital, VIC
- Lina Sharma, Consumer
- David Thomas, Consumer
- Clinical A/Prof Michael Wallace, Department of Hepatology and Western Australian Liver Transplant Service, Sir Charles Gairdner Hospital Medical School, The University of Western Australia, WA
- Prof Desmond Yip, Senior Staff Specialist, Department of Medical Oncology, The Canberra Hospital, ACT
There are many different types of treatment for hepatocellular carcinoma (HCC), which is the most common type of primary liver cancer. Treatment recommended will depend on a range of factors, including:
- the size of the tumour
- how far it has spread within the liver and the body
- whether you have cirrhosis
- if any major blood vessels are involved
- your age and your general health.
A multidisciplinary team (MDT) may meet to discuss the best treatment options for you. Ask your doctor if your case has been discussed by an MDT. Treatments for HCC that affects only the liver include:
- surgery – liver resection or liver transplant
- tumour ablation – heat or alcohol is used to destroy the tumour
- radiation therapy – stereotactic body radiation therapy (SBRT), also known as stereotactic ablative body radiation therapy (SABR), or selective internal radiation therapy (SIRT)
- transarterial chemoembolisation (TACE) – chemotherapy drugs are delivered directly to the tumour via its blood supply.
If the cancer is advanced or has spread beyond the liver, you may be offered drug therapies such as immunotherapy or targeted therapy. Sometimes, if the liver is too damaged, you may be offered palliative treatment.
Before treatment begins, your treatment team may suggest that you exercise, eat a healthy diet, or speak to a counsellor about how you feel. If you smoke, you will be encouraged to stop.
Research shows that quitting smoking before surgery reduces the chance of complications. Preparing for treatment in this way – called 'prehabilitation' – may help your recovery.
Your guide to best cancer care
A lot can happen in a hurry when you’re diagnosed with cancer. The guide to best cancer care for liver cancer can help you make sense of what should happen.
It will help you with what questions to ask your health professionals to make sure you receive the best care at every step.
Read the guide
Surgery
Liver surgery aims to remove all the cancer from the body.
This may be done by removing the part of the liver affected by cancer (liver resection or partial hepatectomy) or by removing the whole liver and replacing it with a liver from a donor (liver transplant).
Your surgeon will talk to you about the most appropriate surgery for you, as well as the risks and any possible complications. There are risks associated with any type of surgery.
A surgeon needs your agreement (consent) before performing the operation. Receiving relevant information about the benefits and risks of surgery before agreeing to it is called informed consent.
Liver resection
The aim of a liver resection is to remove all cancer from the liver, as well as a margin of healthy tissue.
A liver resection is usually performed in a specialist treatment centre. It is suitable for only a small number of people with liver cancer. The liver needs to repair itself after the surgery, so a resection is only an option when the liver is working well.
People with no or early cirrhosis may be considered for surgery, but it is unlikely that people with more advanced cirrhosis will be offered surgery. Surgery is also not suitable for people with ascites or when the cancer has spread to major blood vessels.
Types of liver resection
The surgeon will consider the size and position of the tumour, as well as the health of the liver, to work out how much of the liver can be safely removed.
The liver resection may be called a right or left hepatectomy (removes the right or left part of the liver) or a segmentectomy (removes a small section of the liver).
In some cases, the gall bladder may also be removed, along with part of the muscle that separates the chest from the abdomen (the diaphragm).
If you have a liver resection, it will be carried out under a general anaesthetic. There are two ways to perform the surgery:
- in open surgery, the surgeon makes a large cut in the upper abdomen under the rib cage. This is the most common type of surgery.
- in keyhole (laparoscopic) surgery, the surgeon makes a few small cuts in the abdomen, then inserts a thin instrument with a light and camera (laparoscope) into one of the cuts. Using images from the camera as a guide, the surgeon inserts tools into the other cuts to remove the cancerous tissue.
People who have laparoscopic surgery usually have a shorter stay in hospital, less pain and a faster recovery time. However, laparoscopic surgery is not suitable for everyone with primary liver cancer and it is not available in all hospitals.
Both open surgery and laparoscopic surgery are major operations – talk to your surgeon about the best option for you.
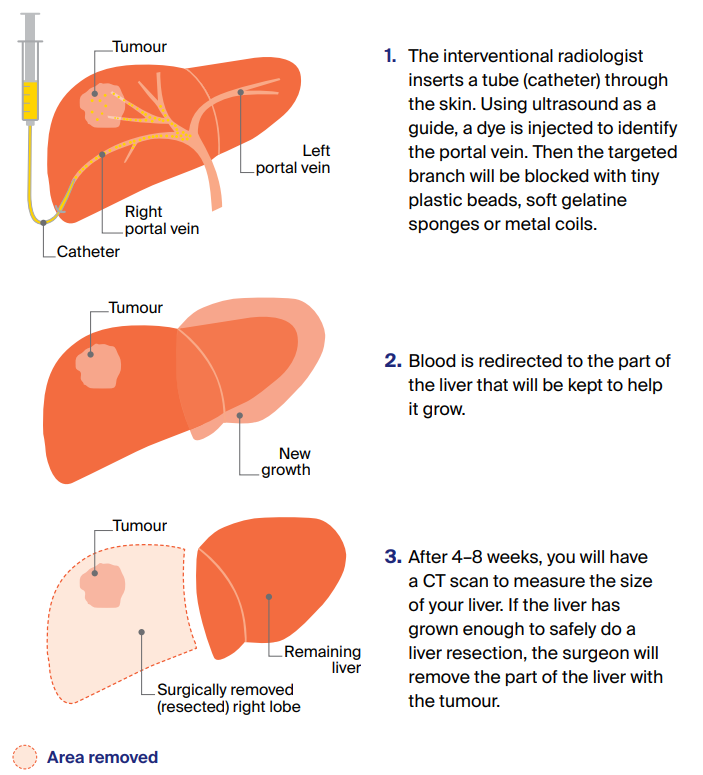
Portal vein embolisation (PVE)
Sometimes, the surgeon needs to remove so much of the liver that the remaining portion may not be large enough to recover. In this case, you may have a portal vein embolisation (PVE) about 4–8 weeks before the liver resection.
A PVE is performed by an interventional radiologist and is normally done under local anaesthetic.
How a PVE is done
In some cases, you may need a portal vein embolisation (PVE) before a liver resection.
A PVE blocks the branch of the portal vein that carries blood to the part of the liver that is going to be surgically removed. Blocking the blood supply allows the other part of the liver to grow bigger.
What to expect after surgery
The portion of the liver that remains after the resection will start to grow, even if up to two-thirds of the liver has been removed. It will usually regrow to its normal size within a few months, although its shape may be slightly changed. After surgery:
- bleeding is a risk because a lot of blood passes through the liver – you will be monitored for signs of bleeding and infection
- some people experience jaundice (yellowing of the skin and whites of the eyes) – this is usually temporary and improves as the liver grows back
- most people will need a high level of care – you will spend 5–10 days in hospital after a liver resection and it is common to spend some time in the high dependency or intensive care unit before moving to a standard room.
Liver transplant
A liver transplant can be an effective treatment for some people with primary liver cancer. It involves removing the whole liver and replacing it with a healthy liver from another person (a donor).
However, liver transplants are suitable for only a small number of people.
Currently, all liver transplants in Australia are performed in public hospitals and there is no cost for in-hospital services. You will usually have to pay for any medicines you continue to take once you leave the hospital.
Transplant eligibility
Those with a single tumour or several small tumours may be able to have a transplant. A liver transplant may also be considered if other therapies such as TACE can shrink the tumour first. This is called downstaging.
To be considered for a liver transplant, you also need to be reasonably fit, not smoke or take illegal drugs, and have stopped drinking alcohol for at least six months.
Liver transplants are not possible when the cancer has spread (metastasised) to other organs or to major blood vessels.
Waiting for a liver transplant
Donor livers are scarce and waiting for a suitable liver may take many months or even several years. During this time, the cancer may continue to grow.
As a result, most people have tumour ablation or TACE to control the cancer while they wait for a donor liver to become available.
Unfortunately, in some people the cancer progresses despite having tumour ablation or TACE, and a liver transplant will no longer be possible.
If this happens, you will be taken off the liver transplant waiting list and your doctor will discuss other treatment options.
What to expect after a transplant
If you have a liver transplant, you will spend up to three weeks in hospital. It may take 3–6 months to recover and it will probably take time to regain your energy.
You will be given medicines called immunosuppressants to stop your body rejecting the new liver. These drugs need to be taken for the rest of your life.
Tumour ablation
For tumours smaller than 3 cm, you may be offered tumour ablation. This destroys the tumour without removing it and may be the best option if you cannot have surgery or are waiting for a transplant.
Ablation can be done in different ways depending on the size, location and shape of the tumour. Thermal ablation and alcohol injection are the most common methods used for liver cancer.
Cryotherapy, which uses freezing to destroy the tumour, is rarely used.
Thermal ablation
This ablation method uses heat to destroy a tumour. The heat may come from radio waves (radiofrequency ablation or RFA) or microwaves (microwave ablation or MWA).
Using an ultrasound or CT scan as a guide, the doctor inserts a fine needle through the abdomen into the liver tumour. The needle sends out radio waves that produce heat and destroy the cancer cells.
Thermal ablation is usually done under general anaesthetic in the x-ray department or the operating theatre. Treatment may take 1–2 hours.
Some people may stay overnight in hospital, but many can leave the hospital after treatment. Side effects may include pain, nausea or fever, but these can be managed with medicines.
Alcohol injection
This ablation method involves injecting pure alcohol (ethanol) into the tumour.
This procedure – called percutaneous ethanol injection or PEI – isn’t available at all hospitals but may be used if other forms of ablation aren’t possible.
For this procedure, a needle is passed into the tumour under local anaesthetic, using an ultrasound as a guide. You may need more than one injection over several sessions.
Side effects are rare but may include pain or fever. These can be managed with medicines.
Radiation therapy
Primary liver cancer is sensitive to radiation but so are healthy liver cells. Two specialised radiation therapy techniques can deliver radiation directly to the tumour while limiting the damage to the healthy part of the liver.
These are called stereotactic body radiation therapy (SBRT) and selective internal radiation therapy (SIRT). SBRT may be suitable for people with early-stage cancer, while SIRT may be offered in more advanced cases.
Conventional external beam radiation therapy (EBRT) is also occasionally used as a palliative treatment to help manage symptoms. For example, short courses of EBRT can help to control pain caused by liver cancer that has spread to the bones.
Stereotactic body radiation therapy (SBRT)
This type of therapy may be called stereotactic body radiation therapy (SBRT) or stereotactic ablative body radiation therapy (SABR). It is a type of EBRT.
The machine precisely targets beams of radiation from many different angles onto the tumour. SBRT is prescribed by a radiation oncologist and delivered in a radiation therapy department.
This method allows a high dose of radiation to be delivered to the tumour while surrounding healthy tissue is protected from the effects of radiation.
SBRT requires fewer treatment sessions than conventional radiation therapy. People may need only 3–8 sessions over one or two weeks.
This treatment may be offered to people with tumours that can’t be removed with surgery or treated with tumour ablation or TACE.
SBRT may also be used to shrink tumours while people are waiting for a liver transplant.
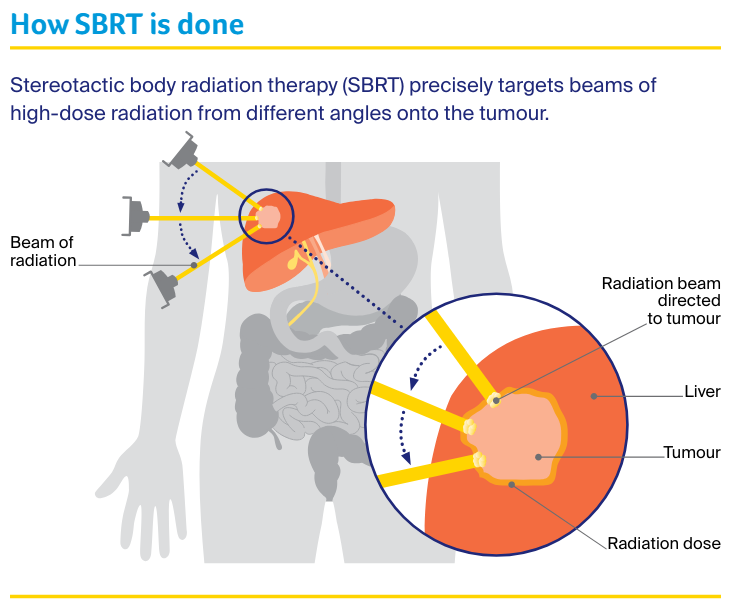
Before this treatment, you will have a CT scan and maybe an MRI scan as well. These scans help make an individual plan for your treatment. You may also need a short procedure to insert small metal markers (called fiducial markers) next to the tumour.
These markers allow the radiation oncologist to monitor the exact position of the tumour during the treatment. They are usually made of gold and are about the size of a grain of rice. A needle is used to put in the markers during the CT scan.
Not all people will need to have these markers inserted. During treatment, you will be asked to lie on a treatment table while a machine delivers the targeted beams to the tumour. It is important to lie very still during SBRT treatment.
Simple breathing techniques – like holding your breath for 10–15 seconds – can help reduce movement during the procedure .Your treatment team will talk to you about this.
SBRT itself is painless, and you can usually go home after the treatment. You will not be radioactive after SBRT.
Selective internal radiation therapy (SIRT)
Selective internal radiation therapy (SIRT) is a different type of radiation therapy.
Sometimes called radioembolisation, SIRT combines embolisation (which blocks blood supply to the tumour) with internal radiation, where the radiation source is placed inside the liver.
In SIRT, the radiation is delivered through the blood vessels to the tumour using tiny radioactive beads, which are made of resin or glass.
The procedure may be offered for primary liver cancer when the tumours can’t be removed with surgery or to shrink tumours before a liver resection or a transplant.
SIRT is performed by an interventional radiologist, supported by a nuclear medicine physician, in a radiology department. One to two weeks before the procedure, you will have a work-up day to ensure the procedure is appropriate for you.
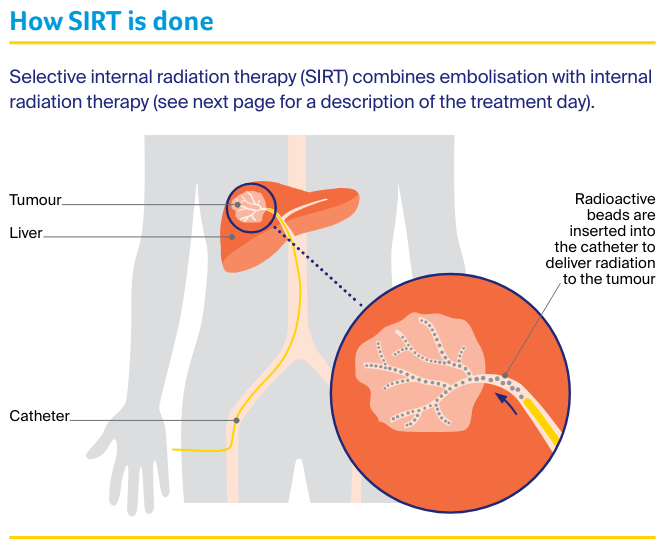
Work-up day – Several tests will be done on this day, including blood tests to check kidney function and blood clotting, and an angiogram (an x-ray of the blood vessels).
Before the angiogram, you will have a local or general anaesthetic. The interventional radiologist will then make a small cut in the groin area and insert a thin plastic tube (called a catheter) into the artery that feeds the liver (hepatic artery).
A small amount of dye will be passed through the catheter into the bloodstream. On an x-ray, the dye provides a detailed map of the blood supply to the liver, which varies from person to person. The doctor may also block some small blood vessels.
This helps to stop the radioactive beads travelling beyond the liver to other parts of the body when you have the SIRT treatment. Next, a substance called a radiotracer will be injected into the catheter and you will have another scan.
This scan shows where the radioactive beads will go on the day of treatment. It will also check if any beads are likely to travel to the lungs. This step helps the doctor work out if it is safe to go ahead with the treatment.
Treatment day – On the day of treatment, you will have another angiogram. The interventional radiologist will make a cut in the groin area and pass a catheter through to the hepatic artery.
The radioactive beads will be inserted through the catheter into the hepatic artery. These beads can then deliver radiation directly to the tumour.
The procedure takes about an hour. You will be monitored after the procedure, and recover in hospital overnight.
After treatment – You may experience flu-like symptoms, nausea and pain, which can be treated with medicines. You can usually go home within 24 hours. The radioactive beads will slowly release radiation into the tumour over the next week or so.
During this time, you may need to take some safety precautions such as avoiding close physical contact with children or pregnant women. You may also be advised to not share a bed or have sex in the first few days after treatment.
“It helps to focus on what is happening now, what is actually known – not all the possibilities. One step at a time.” Sam
Liver cancer clinical trials
Cancer clinical trials are research studies that test whether a new approach to prevention, screening, diagnosis, or treatment works better than current methods and is safe.
There are clinical trials for liver cancer open to recruitment in Victoria. This list shows the most recently updated liver cancer studies on the Victorian Cancer Trials Link (VCTL).
Visit the VCTL to find more liver cancer clinical trials.
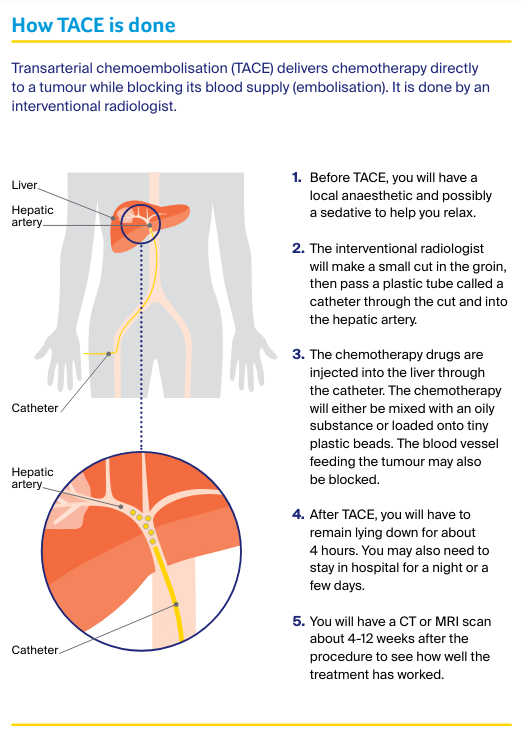
Transarterial chemoembolisation (TACE)
Liver tumours mostly get their blood supply from the hepatic artery. In transarterial chemoembolisation (TACE), chemotherapy is delivered directly to the tumour through this artery.
TACE is usually given to people who can’t have surgery or ablation for primary liver cancer. The procedure may be used to shrink the cancer or stop it growing while people are waiting for a liver transplant or a major liver resection.
It is common to have a fever the day after the procedure, but this usually passes quickly. You may experience nausea and vomiting, or feel some pain, which can be controlled with medicines.
Some people feel tired or have flu-like symptoms for up to a week after the procedure.
“I’d like people with advanced cancer to know that there are a myriad of services. You only have to ask; you are not alone.” Pat
Drug therapies
Two types of drug therapies are available to treat primary liver cancer – immunotherapy and targeted therapy.
Drug therapies (sometimes called systemic therapies) can spread throughout the whole body to treat cancer cells wherever they may be, which can be helpful for cancer that has spread (metastatic cancer).
Drug treatment for advanced liver cancer is changing quickly and new treatments may become available in the near future. You may also be able to get new drugs through clinical trials.
Talk to your doctor about the latest developments and whether there are any suitable clinical trials for you.
Immunotherapy
This is a type of drug treatment that helps the body’s own immune system to fight cancer cells. Immunotherapy drugs known as checkpoint inhibitors block proteins that stop immune cells from recognising and destroying the cancer cells.
Once the proteins are blocked, the immune cells can recognise and attack the cancer.
A checkpoint inhibitor called atezolizumab is the first immunotherapy drug subsidised on the Pharmaceutical Benefits Scheme (PBS) to treat some types of primary liver cancer.
Atezolizumab, which is given in combination with a targeted therapy drug called bevacizumab, is likely to be the first type of drug treatment used.
Immunotherapy drugs are delivered by drip into a vein (intravenously), which may take 1–3 hours. Treatments are usually given every three weeks and your doctor will discuss with you how often and how many treatments will be needed.
Side effects
Immunotherapy can have different side effects for different people. These mostly happen when the immune system becomes overstimulated and attacks organs such as the skin, bowel, liver or hormone-producing glands.
These immune-related side effects can happen when you are having treatment or in the weeks, months, or even years, afterwards. In rare cases, side effects can be the sign of serious complications, so even mild side effects should be reported to your doctor.
Immune-related side effects may need to be treated with drugs to help control the immune response (called immunosuppressive drugs), and the immunotherapy may need to be stopped.
If you are unable to manage the side effects of immunotherapy, your doctor may recommend switching to targeted therapy.
When you start immunotherapy, you may be given an alert card so you can let all health professionals know that you are having this treatment. This ensures that you are given the best treatment if you develop side effects.
Targeted therapy
This type of treatment targets specific features of cancer cells to stop the cancer growing and spreading.
People who have advanced liver cancer and are unable to take immunotherapy may be offered targeted therapy drugs such as sorafenib or lenvatinib. These drugs are both subsidised by the PBS for some types of primary liver cancer.
They are given as tablets that you swallow. Your doctor will explain when to take them. The side effects of sorafenib and lenvatinib may include skin rash, diarrhoea, fatigue and high blood pressure.
These side effects can usually be managed without having to completely stop treatment.
Your treatment team will monitor you while you are taking targeted therapy drugs. If you find the side effects of targeted therapy difficult to manage, your doctor may recommend switching to another drug.
Generally, targeted therapy is continued for as long as there is benefit. If liver cancer progresses despite treatment with sorafenib or lenvatinib, your doctor may talk to you about trying another targeted therapy drug.
Palliative treatment
If liver cancer is advanced when it is first diagnosed or returns after initial treatment, your doctor will discuss treatment options to help control the cancer’s spread and relieve symptoms.
Palliative treatment helps to improve people’s quality of life by managing the symptoms of cancer when a cure is not possible. It is best thought of as supportive care.
Many people think that palliative treatment is for people at the end of their life, but it may help at any stage of advanced liver cancer. It is about living as long as possible in the most satisfying way you can.
Treatment may include radiation therapy, pain management, drainage of fluid or insertion of a stent in the bile duct to relieve jaundice.
Palliative treatment is one aspect of palliative care, in which a team of health professionals aims to meet your physical, emotional, cultural, social and spiritual needs. The team also supports families and carers.
Learn more
Understanding Liver Cancer
Download our Understanding Liver Cancer booklet to learn more and find support.
Download now Order for free