Page last updated: March 2024
The information on this webpage was adapted from Understanding Stomach and Oesophageal Cancers - A guide for people with cancer, their families and friends (2024 edition). This webpage was last updated in March 2024.
Expert content reviewers:
This information was developed based on international clinical practice guidelines, and with the help of a range of health professionals and people affected by these cancers:
- Prof David I Watson, Matthew Flinders Distinguished Professor of Surgery, Flinders University, and Senior Consultant Surgeon, Oesophago-Gastric Surgery Unit, Flinders Medical Centre, SA
- Prof Bryan Burmeister, Senior Radiation Oncologist, GenesisCare Fraser Coast and Hervey Bay Hospital, QLD
- Kieran Cahill, Consumer;
- Jessica Jong, Clinical Dietitian, Upper GI and Hepatobiliary Services, Peter MacCallum Cancer Centre, VIC
- John Leung, Consumer
- Prof Rajvinder Singh, Professor of Medicine, University of Adelaide, and Director, Gastroenterology Department and Head of Endoscopy, Lyell McEwin Hospital, SA
- Dr Sarah Sutherland, Medical Oncologist, Chris O’Brien Lifehouse, NSW
- Paula Swannock, Upper GI Cancer Nurse Consultant, St Vincent’s Hospital Melbourne, VIC
- Rebecca Yeoh, 13 11 20 Consultant, Cancer Council Queensland
The oesophagus and stomach
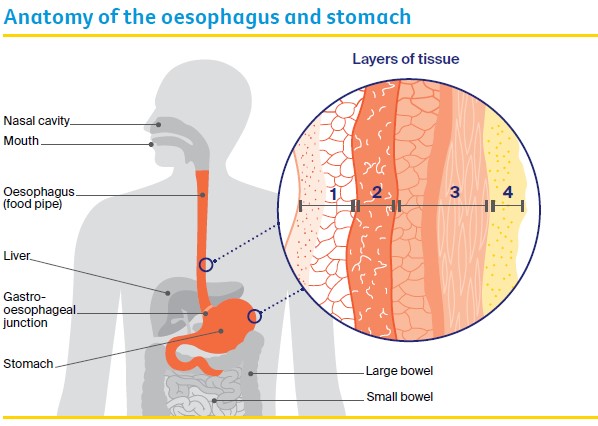
The oesophagus and stomach are part of the upper gastrointestinal (GI) tract, which is part of the digestive system. The digestive system helps the body break down food and turn it into energy.
The oesophagus (food pipe) is a long, muscular tube. The stomach is a hollow, muscular sac-like organ. The top part of the stomach joins to the end of the oesophagus and the other end joins to the beginning of the small bowel.
Stomach cancer
Stomach cancer develops when cells in any part of the stomach grow and divide in an abnormal way.
Tumours can begin anywhere in the stomach, although most start in the stomach’s inner layer (mucosa). This type of cancer is called adenocarcinoma of the stomach (gastric cancer).
If it is not found and treated early, stomach cancer can spread to nearby lymph nodes or to other parts of the body, such as the liver and lungs. It may also spread to the lining of the wall of the abdomen (peritoneum).
Rarely, it can grow through the stomach wall into nearby organs such as the pancreas and bowel.
What the stomach does
The stomach stores food and starts to breaks it down (digests it). Juices and muscle contractions in the stomach break down food into a thick fluid, which then moves into the small bowel.
In the small bowel, nutrients from the broken-down food are absorbed into the bloodstream. The waste moves into the large bowel, where fluids are absorbed into the body and the leftover matter is turned into solid waste (known as faeces).
There are four layers of tissue in the stomach:
- mucosa (moist innermost layer) – made up of glandular cells (column-shaped cells) and produces fluids to help break down food and mucus to protect the stomach lining
- submucosa (supports the mucosa) – provides blood and nutrients to the stomach
- muscle layer – known as the muscularis externa, this layer produces contractions to help break down food and push it into the small bowel
- outer layer – known as the serosa, this layer is a smooth membrane that surrounds the stomach.
Oesophageal cancer
Oesophageal cancer begins when abnormal cells develop in the innermost layer (mucosa) of the oesophagus. A tumour can start anywhere along the oesophagus. There are two main types:
- oesophageal adenocarcinoma – this often starts near the gastro-oesophageal junction and is linked with Barrett’s oesophagus. Adenocarcinomas are the most common form of oesophageal cancer in Australia.
- oesophageal squamous cell carcinoma – this starts in the thin, flat cells of the mucosa, which are called squamous cells. It often begins in the middle and upper part of the oesophagus.
In Australia, oesophageal squamous cell carcinoma is less common than oesophageal adenocarcinoma.
If it is not found and treated early, oesophageal cancer can spread to nearby lymph nodes or to other parts of the body, most commonly the liver and lungs. It can also grow through the oesophageal wall and into nearby organs.
What the oesophagus does
The oesophagus moves food, fluid and saliva from the mouth and throat to the stomach. A valve (sphincter) at the lower end of the oesophagus stops acid and food moving from the stomach back into the oesophagus.
There are four layers of tissue in the oesophagus:
- mucosa (moist innermost layer) – made up of squamous cells (thin, flat cells)
- submucosa (supports the mucosa) – glands in the submucosa make fluid (mucus), which helps to move food through the oesophagus
- muscle layer – known as the muscularis propria, this layer produces contractions to help push food down the oesophagus and into the stomach
- outer layer – known as the adventitia, this layer is connective tissue that supports the oesophagus.
How common are stomach and oesophageal cancers?
About 2580 people are diagnosed with stomach cancer in Australia each year.
Men are almost twice as likely as women to be diagnosed with stomach cancer. It is more common in people over 60, but it can occur at any age.
Stomach cancer statistics
In Australia, about 1740 people are diagnosed with oesophageal cancer each year. Men are much more likely than women to be diagnosed with this cancer.
Oesophageal cancer statistics
Some cancers start at the point where the stomach meets the oesophagus (called the gastro-oesophageal junction). These may be treated similarly to stomach or oesophageal cancer.
Other types of cancer can start in the stomach and oesophagus. These include small cell carcinomas, lymphomas, neuroendocrine tumours and gastrointestinal stromal tumours.
Call Cancer Council 13 11 20 for more information.
Symptoms
Stomach and oesophageal cancers may not cause symptoms in their early stages. Common symptoms can also be caused by many other conditions and do not necessarily mean that you have cancer.
Speak with your general practitioner (GP) if you are concerned.
Common symptoms of stomach cancer
- Unexplained weight loss or loss of appetite
- Difficulty swallowing
- Indigestion – e.g. pain or burning sensation in the abdomen (heartburn), frequent burping, or stomach acid coming back up into the oesophagus (reflux)
- Persistent nausea and/or vomiting (feeling or being sick) with no apparent cause
- Abdominal (belly) pain
- Feeling full after eating even a small amount
- Swelling of the abdomen or feeling bloated
- Unexplained tiredness, which may be due to low red blood cells (anaemia)
- Vomit that has blood in it
- Black or bloody stools.
Common symptoms of oesophageal cancer
- Difficulty swallowing
- New heartburn or reflux
- Reflux that doesn’t go away
- Food or fluids 'catching' in the throat, or episodes of bringing food back up (regurgitation), or vomiting when swallowing
- Pain when swallowing
- Unexplained weight loss or loss of appetite
- Feeling uncomfortable in the upper abdomen, especially when eating
- Unexplained tiredness that won’t go away
- Vomit that has blood in it
- Black or bloody stools (poo).
Risk factors
The exact causes of stomach and oesophageal cancers are not known, however research shows that some factors may increase your risk. Having one or more of these risk factors does not mean you will develop cancer.
Stomach cancer risk factors
- Older age (being over 60)
- Infection with the bacteria Helicobacter pylori (H. pylori)
- Smoking tobacco
- Low red blood cell levels related to pernicious anaemia
- A family history of stomach cancer
- Having an inherited genetic condition like familial adenomatous polyposis (FAP), Lynch syndrome, hereditary diffuse gastric cancer (HDGC), or gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS)
- Chronic inflammation of the stomach (chronic gastritis)
- Carrying extra body weight (overweight or obese)
- Drinking alcohol
- Eating salt-preserved foods (e.g. ham)
- Having a subtotal gastrectomy for a non-cancerous condition.
Oesophageal cancer risk factors
Adenocarcinoma risk factors include:
- carrying extra body weight (overweight or obese)
- medical conditions, including gastro-oesophageal reflux disease (GORD) and Barrett’s oesophagus
- smoking tobacco
- older age (being over 60).
Squamous cell carcinoma risk factors include:
- drinking alcohol
- smoking tobacco
- older age (being over 60)
- damage to the oesophagus from hot or corrosive liquids such as acid.
GORD and Barrett’s oesophagus
Reflux is when stomach acid rises back into the oesophagus. Some people with reflux are diagnosed with gastro-oesophageal reflux disease (GORD).
Over time, stomach acid can damage the lining of the oesophagus and cause inflammation or ulcers (oesophagitis).
This condition is called Barrett’s oesophagus. It only develops in about 1 in 10 people with GORD. In some people, Barrett's oesophagus can lead to the development of oesophageal adenocarcinoma, but this is rare.
If you have Barrett’s oesophagus, your doctor may recommend you have regular endoscopies to look for early changes to the cells that may cause cancer.
Health professionals
Your GP will assess your symptoms and arrange the first tests. You will usually be referred to a specialist such as a gastroenterologist or an upper gastrointestinal surgeon for an endoscopy and further tests.
If you are diagnosed with stomach or oesophageal cancer, the specialist will consider treatment options. Often these will be discussed with other health professionals at what is known as a multidisciplinary team (MDT) meeting.
During and after treatment, you will see a range of health professionals who specialise in different aspects of your care, including a radiation oncologist, speech pathologist and social worker, among others.
Question checklist
Asking your doctor questions will help you make an informed choice. You may want to include some of these questions in your own list.
Diagnosis
- What type of cancer do I have?
- Has the cancer spread? If so, where has it spread? How fast is it growing?
- Are the latest tests and treatments for this cancer available in this hospital?
- Will a multidisciplinary team be involved in my care?
- Are there clinical guidelines for this type of cancer?
Treatment
- What treatment do you recommend? What is the aim of the treatment?
- Are there other treatment choices for me? If not, why not?
- If I don’t have the treatment, what should I expect?
- How long do I have to make a decision?
- I’m thinking of getting a second opinion. Can you recommend anyone?
- How long will treatment take? Will I have to stay in hospital?
- Are there any out-of-pocket expenses not covered by Medicare or my private health cover? Can the cost be reduced if I can’t afford it?
- How will I know if the treatment is working?
- Are there any clinical trials or research studies I could join?
Side effects
- What are the risks and possible side effects of each treatment?
- Will I have a lot of pain? What will be done about this?
- Can I work, drive and do my normal activities while having treatment?
- Will the treatment affect my sex life and fertility?
- How will the treatment affect the way I eat and digest food?
- Can you refer me to a dietitian and/or speech pathologist to help me with eating?
- Are there any complementary therapies that might help me?
After treatment
- How often will I need check-ups after treatment? Who should I see?
- If the cancer returns, how will I know? What treatments could I have?
Understanding Stomach and Oesophageal Cancers
Download our Understanding Stomach and Oesophageal Cancers booklet to learn more.
Download now Order for free