If you’re 25 or older and have a cervix, you need a Cervical Screening Test every five years. The Cervical Screening Test detects HPV, which if left untreated, could lead to cervical cancer. This test is your best protection against cervical cancer.
Before you’ve had your test, you may have questions about what the test involves and what happens next. That’s pretty normal – there’s still some misconceptions out there. It’s useful to ask questions during the appointment, your cervical screening provider will be able to explain all of this for you.
What you’ll find in this article:
So, what’s it like having a Cervical Screening Test?
Robyn, aged 26, shares her experience
Going for my first Cervical Screening Test, I felt nervous and a little anxious. I was scared about what was going to happen and what was expected of me.
I called ahead and made an appointment with a female practitioner as this helped me to feel more comfortable, knowing that they would be able to relate to my experience.
During my appointment, I asked lots of questions about the procedure. I think this helped to put my mind at ease.
It was a little uncomfortable, but it did not hurt me. After, I felt so proud of myself for going to my appointment, staying calm and pushing through. It really wasn’t as bad as what I thought it would be.
My advice to others is – do some research, have a look online about what to expect and what happens at a cervical screening appointment.
On the day of your appointment, try to stay as calm as possible, wear loose clothing and use the toilet beforehand so you don’t have a full bladder!
If you’re aged 25 to 74 and have a cervix, you need to have a Cervical Screening Test every five years. This test offers your best protection against cervical cancer.
After you’ve had your test here’s what comes next.
Your Cervical Screening Test results explained
The Cervical Screening Test looks for the presence of HPV or Human Papillomavirus. Around 80% of people have HPV at some point in their lives but may never know as there are usually no symptoms.
HPV is passed on by genital skin-to-skin contact and can infect all genders and gender diverse people. It is not passed on by blood, semen or saliva.
There are over 100 different types of HPV, but there are a few high-risk types, including types 16 and 18, that are linked with cervical cancer.
The body can get rid of most types of HPV naturally, but if it doesn’t get rid of a high-risk type, they can cause changes to the cells in your cervix. If these cell changes are not picked up early and treated, they could turn into cervical cancer.
Most people who have a Cervical Screening Test will receive a negative result, meaning that HPV was not detected. A small proportion of people will receive a positive result, meaning that some type of HPV was detected.
Even if HPV is detected it’s important to remember that an HPV infection can take about 10-15 years to develop into cancer. If you test positive for HPV it does not mean you have cervical cancer. Your doctor can explain the next steps and arrange appropriate follow up tests, such as a colposcopy .
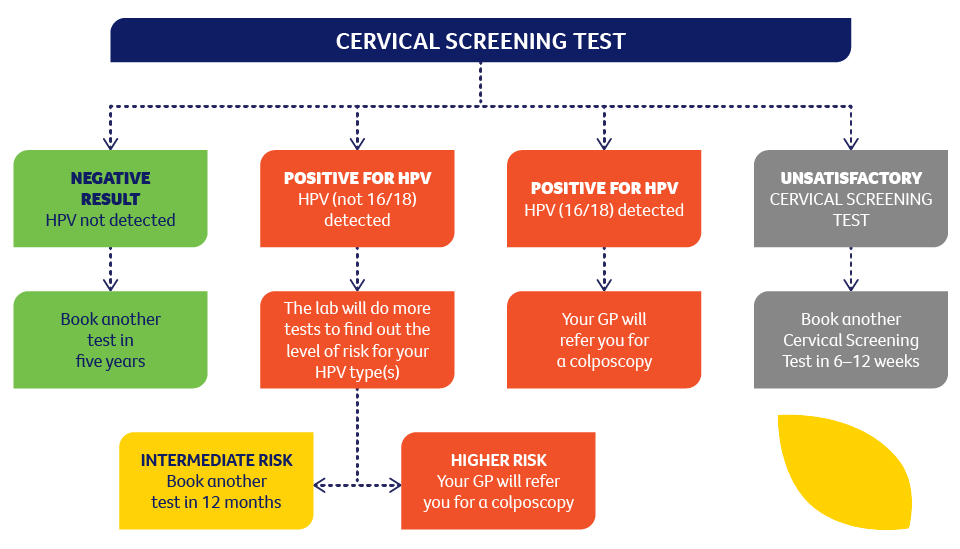
The following diagram explains what happens after your Cervical Screening Test
So, what is a colposcopy?
If your Cervical Screening Test shows that you have tested positive for HPV types that need further investigation and/or that you have abnormal cells that may need treatment, you will be referred to a specialist for a colposcopy. This does not mean that you have cervical cancer.
A colposcopy is a procedure that feels like having a Cervical Screening Test and involves the specialist looking at the cells of the cervix more closely. A colposcopy generally takes 10–15 minutes and the doctor may decide to take a sample of tissue (a biopsy) from the cervix for further testing.
Want to hear from someone whose been through it? Here’s Lena who at age 32 required a colposcopy.

“The colposcopy feels a bit like a cervical screen. It was all over in about 15 minutes – it was very cool to see what my cervix actually looks like on a TV screen.”
I always had my results come back negative, but then in 2019 I was diagnosed with HPV, which can potentially lead to cervical cancer. I remember feeling a rollercoaster of emotions: I felt scared and confused because I had received the HPV vaccine as a teenager.
My GP explained that the HPV vaccine only covers certain strains of HPV (of which there are many!) which is why I still managed to pick it up despite being vaccinated. She reiterated how common HPV is, and that the fact that I have non-16/18 means it is less likely to develop into cancer than the 16/18 strains. She also said that there’s a good chance my body would clear the HPV infection up on its own, but if not, the treatment is straightforward. This put my mind at ease.
I went on to have a colposcopy, I was anxious in the lead up to that test. I was seen by a specialist in the public system who was amazing – they explained the process clearly, and we were just chatting away during the procedure.
The colposcopy feels like a cervical screen, the specialist just spends more time down there! And you can see on a TV what they see – which I found very cool to see what my cervix actually looks like. It was all over in about 15 minutes – luckily there were no abnormalities on my cervix but I was told I would need to go back to my GP for a Cervical Screening Test in 12 months.
“HPV is a pretty normal part of being sexually active”
It is interesting that when I’ve shared my experience with friends, how many say they’ve also had HPV and a colposcopy, and even had to go on for further treatment. It just goes to show how HPV is a pretty normal part of being sexually active, and how easily treatable it is – but also how important it is to get screened to prevent cervical cancer.
Here are three things to remember:
-
Screening is the best protection against cervical cancer. Globally, cervical cancer is the fourth most common cancer among women, yet it is a largely preventable condition. Regular cervical screening is your best protection against cervical cancer.
-
You have a choice. You can book a Cervical Screening Test with any health care provider who does cervical screening – nurses, GPs, gynaecologists. There are choices available. Visit our director y of cervical screening providers across Victoria to find one that meets your needs.
-
A better test, less often. In December 2017, cervical screening changed in Australia. The two-yearly Pap test was replaced with a five-yearly Cervical Screening Test. The new test looks for HPV – the main cause of cervical cancer and is just as safe and more effective than the old Pap test.
To find out more about Cervical Screening, visit: cancervic.org.au/at-your-cervix . You’ll also be able to find a cervical screening provider to suit you and your needs.