The uterus
 The female reproductive system
The female reproductive system
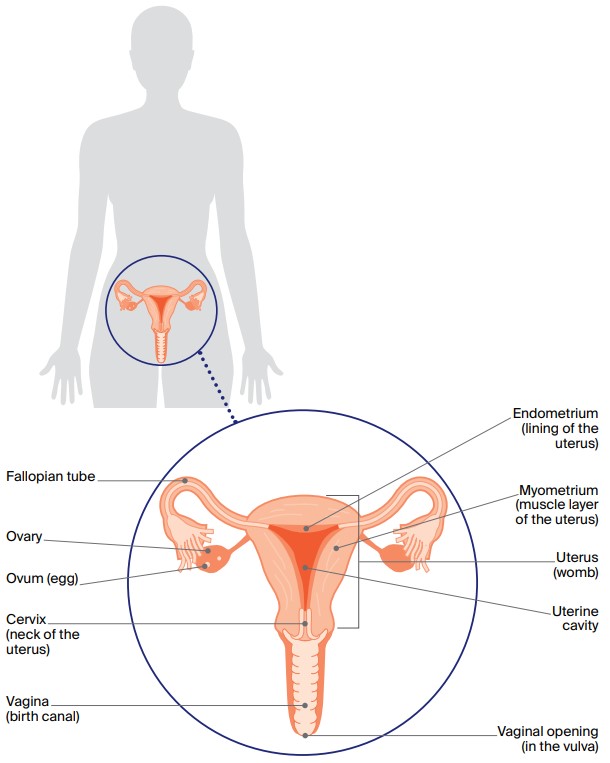
The uterus, or womb, is where a baby grows during pregnancy. It is about the size and shape of a hollow, upside-down pear.
The uterus is part of the female reproductive system, which also includes the ovaries, fallopian tubes, cervix (neck of the uterus), vagina (birth canal) and vulva (external genitals). It sits low in the abdomen (belly), between the bladder and rectum, and is joined to the vagina by the cervix. On either side of the uterus are the ovaries, which contain eggs (ova). The ovaries are connected to the uterus by the fallopian tubes.
The uterus has two layers. The myometrium is the outer layer of muscle tissue and makes up most of the uterus, and the endometrium is the inner layer or lining. Each month, from puberty to menopause, the endometrium becomes thicker to prepare for pregnancy. If a pregnancy does not occur, some of the lining is shed and flows out of the body through the vagina in what is called monthly period or menstruation.
The hormones oestrogen and progesterone control the release of eggs (ovulation) and the timing of menstruation. As you get older, the ovaries gradually produce less of these hormones. When the levels of oestrogen and progesterone fall low enough, periods become irregular and finally stop. This is known as menopause. After menopause, it is not possible to conceive a child naturally. The uterus also becomes smaller and the endometrium becomes thinner.
Your guide to best cancer care
A lot can happen in a hurry when you’re diagnosed with cancer. The guide to best cancer care for endometrial cancer can help you make sense of what should happen. It will help you with what questions to ask your health professionals to make sure you receive the best care at every step.
Read the guide
Types of cancer of the uterus
Cancer of the uterus (also called uterine cancer) occurs when cells in any part of the uterus become abnormal, grow out of control and form a lump (tumour). It can be either endometrial cancer (around 95% of all uterine cancers) or the less common uterine sarcoma: (around 5% of all uterine cancers).
Endometrial cancer
This cancer begins in the cells in the lining of the uterus (called the endometrium).
Endometrial cancer was traditionally categorised as type 1 (linked to excess oestrogen) or type 2 (not linked to oestrogen). With advances in testing and treatment, however, endometrial cancer is increasingly being categorised according to 4 subtypes based on the particular gene changes in the cancer cells.
Tests on tissue samples collected during surgery look for gene changes and help the doctor to work out the subtype of endometrial cancer and what treatment may be needed after surgery. Talk to your doctor about these tests.
Uterine sarcomas
These are rare soft tissue sarcomas that develop in the cells in the muscle of the uterus (myometrium) or the connective tissue (stroma). There are three types:
- endometrial stromal
- leiomyosarcoma
- undifferentiated
Other uterine conditions
Some conditions can affect the uterus and cause abnormal vaginal bleeding and pain. They may be found during tests for cancer of the uterus and can be treated in different ways including surgery and hormones.
- Polyps – Small, soft growths attached to the inner wall of the uterus. Polyps are usually benign (not cancer), although some may eventually turn into cancer.
- Fibroids – Benign tumours that begin in the muscle layer of the uterus (myometrium).
- Endometrial hyperplasia – Thickening of the lining of the uterus (endometrium) caused by too much oestrogen. It is usually benign, but in some cases can lead to cancer.
- Endometriosis – When endometrial tissue grows outside the uterus, e.g. in the abdomen. It doesn’t lead to cancer, but many people also have endometrial hyperplasia.
Symptoms
The most common symptom of cancer of the uterus is unusual vaginal bleeding. This may include:
- bleeding or spotting after menopause
- heavier than usual periods or other changes in periods
- bleeding between periods
- constant bleeding (periods that continue without a break).
A less common symptom is a smelly, watery vaginal discharge. In rare cases, symptoms include abdominal pain, unexplained weight loss, difficulty urinating (weeing) or a change in bowel habit (pooing). Any of these symptoms can happen for other reasons, but it is best to see your doctor for a check-up.
How common is it?
Each year, about 3,300 Australian women are diagnosed with cancer of the uterus, and most are over 50. It is the fifth most common cancer in women and the most commonly diagnosed gynaecological cancer in Australia.
The number of women diagnosed with cancer of the uterus has increased in recent years, and includes younger women. This increase is likely to be linked to rising rates of obesity and diabetes, as well as more people living to older ages.
Anyone with a uterus can get cancer of the uterus – women, transgender men, non-binary people and people with intersex variations.
Risk factors
The exact cause of cancer of the uterus is unknown, but factors that can increase the risk include:
- age – uterine cancer is most common in women over 50 and in women who have stopped having periods (postmenopausal).
- body weight – being overweight or obese is a major risk factor.
- medical factors – including having diabetes, having previous pelvic radiation therapy for cancer and having endometrial hyperplasia.
- family history – having one or more close blood relatives diagnosed with uterine or ovarian cancer, or inheriting a genetic condition such as Lynch syndrome or Cowden syndrome.
- reproductive history – not having children.
- hormonal factors – including starting periods before the age of 12, going through menopause after the age of 55, taking some types of oestrogen-only menopause hormone therapy (MHT) or taking tamoxifen, an anti-oestrogen drug used for breast cancer.
Many women who have risk factors don’t develop cancer of the uterus, and some women who get this cancer have no risk factors. Maintaining a healthy body weight and being physically active are the best ways to reduce the risk of developing cancer of the uterus.
Health professionals
Your general practitioner (GP) will arrange the first tests to assess any symptoms. If these tests do not rule out cancer, you will be referred to a gynaecological oncologist or gynaecologist for more tests. If cancer of the uterus is diagnosed, the specialist will consider treatment options. To ensure the best outcome, it is recommended that you are treated by a specialist gynaecological cancer team.
Treatment options will often be discussed with other health professionals at what is known as a multidisciplinary team (MDT) meeting. During and after treatment, you may see a range of health professionals for various aspects of your care.
Health professionals you may see
- gynaecological oncologist: diagnoses and performs surgery for cancers of the female reproductive system (e.g. cancer of the uterus, or cervical, ovarian, vulvar and vaginal cancers)
- gynaecologist: specialises in diseases of the female reproductive system; may diagnose cancer of the uterus and then refer you to a gynaecological oncologist
- radiation oncologist: treats cancer by prescribing and overseeing a course of radiation therapy
- medical oncologist: treats cancer with drug therapies such as chemotherapy, hormone therapy, targeted therapy and immunotherapy (systemic treatment)
- cancer genetics specialist: specialises in understanding cancers that have occurred as a result of inherited risk
- cancer care coordinator: coordinates your care, liaises with other members of the MDT and supports you and your family throughout treatment; care may also be coordinated by a clinical nurse consultant (CNC) or clinical nurse specialist (CNS)
- nurse: administers drugs and provides care, information and support throughout treatment
- fertility specialist: diagnoses, treats and manages infertility; may be an obstetrician, gynaecologist or reproductive endocrinologist
- women’s health physiotherapist: assists with physical problems associated with gynaecological cancers, such as bladder and bowel issues, sexual issues and pelvic pain
- lymphoedema practitioner: educates people about lymphoedema prevention and management, and provides treatment if lymphoedema occurs; often a physiotherapist or occupational therapist
- psychologist, counsellor: help you manage your emotional response to diagnosis and treatment
Understanding Cancer of the Uterus
Download our Understanding Cancer of the Uterus booklet to learn more and find support
Download now Order for free
Expert content reviewers:
A/Prof Orla McNally, Consultant Gynaecological Oncologist, Director Oncology/Dysplasia, Royal Women’s Hospital, Honorary Clinical Associate Professor, University of Melbourne, and Director of Gynaecology Tumour Stream, Victorian Comprehensive Cancer Centre, VIC; A/Prof Yoland Antill, Medical Oncologist, Peninsula Health, Parkville Familial Cancer Centre, Cabrini Health and Monash University, VIC; Grace Guerzoni, Consumer; Zeina Hayes, 13 11 20 Consultant, Cancer Council Victoria; Bronwyn Jennings, Gynaecology Oncology Clinical Nurse Consultant, Mater Hospital Brisbane, QLD; A/Prof Christopher Milross, Director of Mission and Radiation Oncologist, Chris O’Brien Lifehouse, NSW; Mariad O’Gorman, Clinical Psychologist, Liverpool Cancer Therapy Centre and Bankstown Cancer Centre, NSW
Page last updated:
The information on this webpage was adapted from Understanding Cancer of the Uterus - A guide for people with cancer, their families and friends (2023 edition). This webpage was last updated in November 2023.