What is penile cancer?
Penile cancer is a rare type of cancer that occurs on the foreskin, the glans (head) of the penis, or on the skin of the penile shaft. It occurs mostly in uncircumcised men (men who still have foreskin around the head of the penis).
Sometimes growths can develop on the penis that are abnormal but are not malignant (these are called benign tumours). These lesions look like warts or irritated patches of the skin. These can be caused by the human papillomavirus (HPV) and may increase your risk of penile cancer.
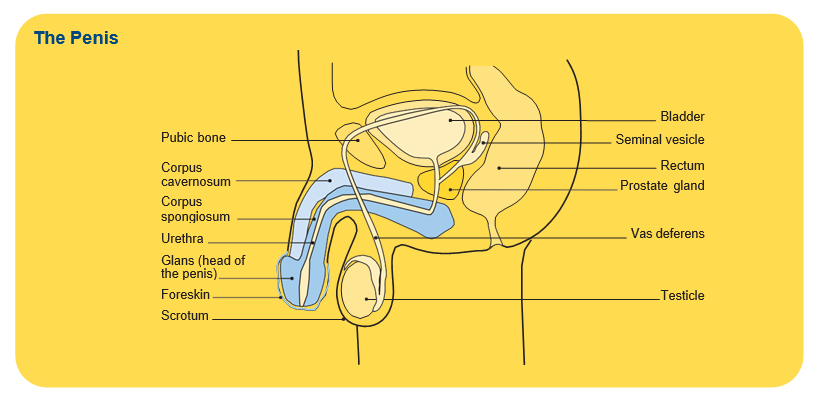
The penis
The penis is the male external sex organ. It is also part of the urinary system. It is made up of different types of tissue such as skin, muscle, nerves and blood vessels. During sexual arousal, blood flows into the chambers of the penis and makes it hard and erect.
The penis also contains the urethra, a thin tube that carries urine from the bladder and semen from the testicles out of the body.
Types of penile cancer
There are several types of penile cancer, depending on the type of cell from which the cancer develops. Almost all penile cancers start in the surface layer of cells (epithelium) of the penis.
- Squamous cell cancer (SCC) – the most common type of penile cancer, accounting for around 95% of cases. Most of this type of cancer start on the foreskin (in men that have not been circumcised) or on the head of the penis (glans), but it can occur on the penile skin of the shaft as well.
- Carcinoma in situ (CIS), penile intraepithelial neoplasia (PeIN) – the earliest stage of squamous cell penile cancer where cancer cells are only found in the very top layer of the skin cells, and the cancer has not spread any deeper.
Other rarer types of penile cancer include:
- Basal cell carcinoma (BCC) – another type of skin cancer that can develop in deeper cells of the squamous cells in a layer of skin.
- Adenocarcinoma – a type of cancer that develops in the sweat glands in the skin of the penis.
- Melanoma of the penis – a type of cancer that develops in the pigmented skin cells that give the skin its colour.
- Penile sarcoma – a very rare type of cancer that develops in the deeper tissues of the penis such as the blood vessels, muscle, fat or connective tissue.
How common is penile cancer?
Penile cancer is rare with around 103 Australians diagnosed each year (about 0.8 cases per 100,000 people). It is more likely to be diagnosed in men over 50 years old but can also occur in younger men.
Learn more about rare cancer
Risk factors
The cause of penile cancer is not known in most cases. However, there are several risk factors, including:
- Human papillomavirus (HPV) infection – this common group of viruses are spread through sexual contact. Most people with HPV do not develop cancer but HPV infection is found in about half of all penile cancers. Some types of HPV can cause genital warts, which increase the risk of developing penile cancer.
- Not being circumcised – penile cancer is more common in men who are not circumcised. Circumcision is the surgical removal of the foreskin that covers the end of the penis. Men who have a tight foreskin that is hard to pull back (phimosis) for washing sometimes notice a secretion under the foreskin that becomes a smelly substance (smegma). While smegma doesn’t necessarily cause penile cancer, it can irritate and inflame the penis, which can increase the risk of cancer.
- Smoking – chemicals found in cigarettes and other forms of tobacco can damage cells in the body, including cells in the penis, which can increase your risk of developing penile cancer.
- Age – the risk of penile cancer increases with age and is more common in men over 50 years old.
- Certain skin conditions – men who have skin conditions such as psoriasis or lichen sclerosus may have a higher rate of penile cancer.
- HIV/AIDS – infection with the human immunodeficiency virus (HIV) causes acquired immune deficiency syndrome (AIDS) and men who contract HIV have a greater risk of developing penile cancer as their immune system is less able to fight off cancer.
- Premalignant lesions/conditions – if left untreated, these can become cancerous.
- Exposure to ultraviolet (UV) radiation – from either sunlight or UV lamps.
Symptoms
People with penile cancer may experience a range of different symptoms including:
- a growth or sore on the head of the penis (the glans), the foreskin or the shaft of the penis that doesn’t heal in a couple of weeks
- bleeding from the penis or under the foreskin
- a smelly discharge under the foreskin
- a hard lump under the foreskin
- changes in the colour of the skin on the penis or foreskin
- thickening of the skin on the penis or foreskin that makes it difficult to pull back the foreskin
- pain in the shaft or tip of the penis
- swelling at the tip of the penis
- a rash on the penis or a persistent red patch of skin that does not go away
- lumps in the groin due to swollen lymph nodes.
Having any of these symptoms does not mean you have penile cancer, but if you experience any of these symptoms you need to discuss them with your doctor.
Diagnosis
If your doctor thinks that you may have penile cancer, they will talk to you about your medical history, perform a physical examination and suggest that you have certain tests, which may include:
- Blood tests – a full blood count, tumour markers (to measure chemicals produced by cancer cells) and to check if you have an infection.
- Biopsy – the removal of some tissue from the affected area or region for examination under a microscope. In penile cancer, you may have a punch biopsy or elliptical excision, a fine needle aspiration biopsy, a sentinel lymph node biopsy or a removal of the lymph nodes.
- Ultrasound scan – high-frequency soundwaves are used to create pictures of the inside of your body.
- CT (computerised tomography) or MRI (magnetic resonance imaging) scans – special painless machines are used to scan and create pictures of the inside of your body.
- PET (positron emission tomography)–CT scan – a scan combined with a CT scan where you are injected with a glucose solution containing some radioactive material, which helps cancer cells show up brighter on the scan.
Finding a specialist
You can utilise Rare Cancers Australia's directory of health professionals and cancer services across Australia for further resources and information about penile cancer.
Visit Rare Cancers Australia
Grading and staging
If cancer cells are found during any of your tests, your doctor will need to know the tumour grade and stage so your team of health professionals can develop the best treatment plan for you. The grade of the cancer lets your doctor know how quickly the cancer might grow and spread, while the stage of the cancer describes its size and whether it has spread.
Penile cancer is graded from 1 to 3, with 1 being the lowest grade and 3 being the highest grade. Low-grade means that the cancer cells are slow growing and less likely to spread. High-grade means that the cancer cells grow more quickly and are more likely to spread. There are several staging systems for penile cancer, but the one most commonly used is the TNM (tumour-nodes-metastasis) staging system.
Understanding Penile Cancer
Download our Understanding Penile Cancer fact sheet to learn more.
Download now
Expert content reviewers:
Gregory Bock, Urology Cancer Nurse Coordinator, WA Cancer and Palliative Care Network, North Metropolitan Health Service, WA; Dr Mikhail Lozinskiy, Consultant Urologist, Royal Perth Hospital, WA; Caitriona Nienaber, 13 11 20 Consultant, Cancer Council WA; Prof Manish Patel, Urological cancer surgeon, University of Sydney, Westmead and Macquarie University Hospitals, Sydney, NSW; Walter Wood, Consumer; Dr Carlo Yuen, Urologist, St Vincent’s Hospital, Sydney, Conjoint Senior Lecturer UNSW.
Page last updated:
The information on this webpage was adapted from Understanding Penile Cancer - A guide for people affected by cancer (2021 edition). This webpage was last updated in June 2021.