Treatment options by type of bowel cancer
Colon cancer and rectal cancer are treated differently. Your health care team will recommend treatment based on what will give you the best outcome, where the cancer is in the bowel, whether and how the cancer has spread, your general health, and your preferences.
Colon cancer
- Surgery is the main treatment for early and locally advanced colon cancer.
- If the cancer has spread to the lymph nodes, you may have chemotherapy after surgery, which is called adjuvant chemotherapy.
- Radiation therapy is not used for early colon cancer.
Rectal cancer
- Surgery is the main treatment for early rectal cancer.
- If the cancer has spread beyond the rectal wall and/or into nearby lymph nodes, before surgery you will have chemotherapy or radiation therapy combined with chemotherapy (chemoradiation).
- After surgery you may have further chemotherapy or radiation therapy. Trials are looking at other combinations of chemotherapy and radiation therapy.
You may be given iron as tablets or injections to increase your iron levels and blood count before starting treatment. You may also have a changed diet to limit weight loss and improve your strength, reduce blockages and make having bowel movements easier. If you are a smoker, you will be encouraged to stop smoking before surgery.
Your guide to best cancer care
A lot can happen in a hurry when you’re diagnosed with cancer. The guide to best cancer care for bowel cancer can help you make sense of what should happen. It will help you with what questions to ask your health professionals to make sure you receive the best care at every step.
Read the guide
Surgery
The aim of surgery is to remove as much of the cancer as possible and nearby lymph nodes. There are two ways to perform surgery for bowel cancer:
- Keyhole surgery – involves several small cuts (incisions) in the abdomen, through which long, thin instruments are inserted to remove the section of bowel with the cancer. Keyhole surgery usually means less pain and scarring, a shorter hospital stay and faster recovery.
- Open surgery – usually done with one long cut down the middle of your abdomen. Open surgery usually means a larger wound, slower recovery and a longer hospital stay.
Surgery for cancer in the colon
The most common type of surgery for colon cancer is a colectomy (removal of a part of the bowel). Lymph nodes near the colon and some normal bowel around the cancer will also be removed.
The surgeon usually cuts the bowel on either side of the cancer, with a small border of healthy tissue called the margin, and then joins the two ends of the bowel back together. This join is called an anastomosis.
Sometimes one end of the bowel is brought through an opening made in your abdomen and stitched onto the skin. This procedure is called a colostomy (if made from the large bowel) or ileostomy (if made from the small bowel). The opening – called a stoma – allows faeces to be collected in a bag.
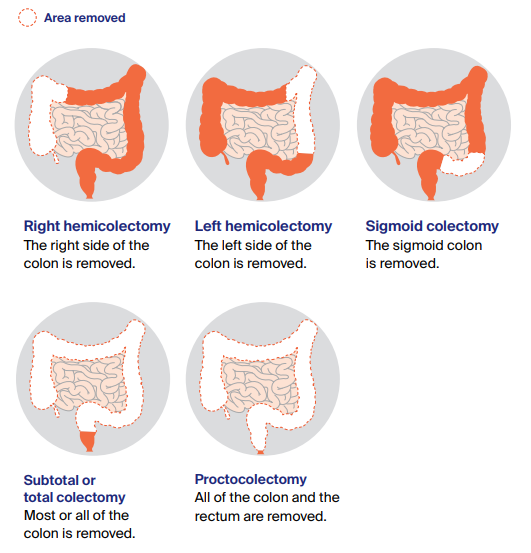
Types of colectomies
There are different types of colectomies depending on which part of the colon is removed. The surgery may be done as keyhole or open surgery.
Surgery for cancer in the rectum
Surgery for cancer in the rectum depends on where the cancer is located, whether the bowel can be rejoined, and where in the rectum the join can be made. The surgery may be performed using an open or keyhole approach.
There are different types of operation, but the two most common include:
- Anterior resection – this is the most common operation. It may include creating a temporary stoma, which will be reversed later.
- Abdominoperineal resection – this procedure may be recommended if the cancer is near the anal sphincter muscles or if it is too low to be removed without causing incontinence (loss of control over bowel movements). After an abdominoperineal resection, you will need a permanent stoma.
Other types of surgery
Local excision
People who have very early-stage rectal cancer or are not fit for a major operation may have a local excision. The surgeon inserts an instrument into the anus to remove the cancer from the lining of the rectum, along with a margin of healthy tissue, without cutting into the abdomen.
If there are two cancers
In a small number of people, two separate cancers may be found in the large bowel at the same time. The cancers may be discovered through diagnostic tests or during surgery. In this case, there are several options for surgery:
- remove two sections of the bowel
- remove one larger section of the bowel, which includes both areas with cancer
- remove the entire colon and rectum (proctocolectomy) to prevent any chance of another cancer forming.
Surgery for a blocked bowel
Sometimes as the bowel cancer grows, it completely blocks the bowel, which is called a bowel obstruction. Waste matter cannot pass through the blocked bowel easily, and may cause bloating and abdominal pain, constipation, nausea and vomiting.
Sometimes the obstruction is found and cleared during the surgery to remove the cancer. In other cases, the bowel obstruction will mean you have to have emergency surgery to clear the blockage. It may be possible to rejoin the bowel during the surgery, but some people may need a stoma.
Not everyone with a blockage will want to have surgery or be fit enough to have it. To help keep the bowel open so that stools can pass through again, your surgeon may be able to insert a small hollow tube (stent) inside the colon. A stent may also help manage the blockage until you are well enough to have an operation.
If you are unable to have surgery or a stent, you may be given medicine to help control the symptoms of a bowel obstruction.
What to expect after surgery
As with any major operation, bowel surgery has risks. Complications may include infection, bleeding, blood clots, damage to nearby organs, or leaking from the joins between the removed parts of the bowel.
Your recovery time after the operation will depend on your age, whether you had keyhole or open surgery and your general health. You will probably be in hospital for 4–7 days, but it can take 2–3 months to fully recover.
Side effect of bowel surgery can include changes in bowel function, changes in sexual function, changes to your diet, fatigue and a temporary or permanent stoma.
Radiation therapy
Radiation therapy uses a controlled dose of radiation, such as focused x-ray beams, to kill or damage cancer cells. It is often combined with chemotherapy (chemoradiation). This is because chemotherapy makes cancer cells more sensitive to radiation.
Radiation therapy may be recommended for rectal cancer but is not generally used to treat colon cancer. It is given:
- before surgery (neoadjuvant) – radiation therapy is used before surgery to shrink the tumour. This makes it easier for the surgeon to completely remove the cancer and also reduces the risk of the cancer coming back.
- after surgery (adjuvant) – occasionally, if the rectal cancer is found to be more advanced than originally thought, radiation therapy may be used after surgery to destroy any remaining cancer cells. This only happens if radiation therapy was not given before surgery.
External beam radiation therapy is the most common type of radiation therapy for rectal cancer. Newer technology means that treatment machines can accurately deliver a high dose to the affected area, with much lower doses going to the surrounding tissue. This helps to reduce the side effects from radiation therapy.
You will have more imaging scans to help your radiation oncologist design a treatment plan for your situation. This will include the number of sessions you’ll have and whether you will also have chemotherapy.
Before treatment, some small marks like a freckle may be tattooed on your skin to help pinpoint the exact area to receive the radiation. Treatment is given daily on weekdays. During treatment, you will lie on a treatment table under a machine called a linear accelerator. Each treatment takes only a few minutes, but a session may last 10–20 minutes because of the time it takes to set up the machine. The treatment is painless and can’t be seen or felt.
After finishing your neoadjuvant treatment, there will be a break before surgery. This gives time for the radiation therapy to have its full effect.
Most side effects are temporary and disappear a few weeks or months after treatment. Common side effects include tiredness, and irritation to the bowel and bladder. This may mean needing to pass urine more often, experience a burning sensation when you pass urine, experinece redness or soreness in the treatment area, faecal urgency and incontinence, diarrhoea, constipation, and mucus discharge or small amounts of bleeding from the anus. Radiation therapy can cause the skin or internal tissue to become less stretchy and harden (fibrosis). It can also inflame the lining of the rectum.
Effects on fertility and sexual function
Radiation therapy to the pelvis and rectum can affect your sexual function and ability to have children (fertility). Speaking to a counsellor about your feelings can be helpful. You can also call Cancer Council on 13 11 20 to talk to a health professional about your concerns.
For men
Radiation therapy can temporarily or permanently damage sperm or reduce sperm production. Talk to your doctor about storing sperm at a hospital or fertility clinic if you are thinking of having children in the future. Radiation therapy can also damage blood vessels and nerves that produce erections, which may cause some men may have erection problems.
Learn more about sexuality and intimacy
For women
Radiation therapy can cause the vagina to become shorter and narrower, making sexual intercourse painful. Your doctor may suggest using a vaginal dilator after treatment ends and the area has healed to help gradually widen the entrance and prevent the side walls sticking together.
In some cases, radiation therapy can stop the ovaries producing female hormones, which can cause menopause. After menopause you will not be able to conceive a child.
Learn more about fertility
Chemotherapy
Chemotherapy uses drugs to kill or slow the growth of cancer cells while doing the least possible damage to healthy cells. You will probably have chemotherapy as a course of several sessions (cycles) over 4 to 6 months.
If the cancer has spread outside the bowel to lymph nodes or to other organs, chemotherapy may be recommended:
- Before surgery (neoadjuvant) – to shrink the tumour and make it easier to remove. You are likely to have chemotherapy together with radiation therapy (chemoradiation) for rectal cancer.
- After surgery (adjuvant) – for either colon or rectal cancer to kill any remaining cancer cells and reduce the chance of the cancer coming back. If your doctor recommends chemotherapy, you will probably start treatment within 6 to 8 weeks.
- On its own – if the cancer has spread to other organs, such as the liver or lungs, chemotherapy may be used either to shrink the tumours or to reduce symptoms and make you more comfortable.
Common side effects of chemotherapy include tiredness, nausea and vomiting, diarrhoea, mouth sores and ulcers, changes in appetite, taste and smell, sore hands and feet, and hair loss or thinning. You may also be more likely to catch infections.
Understanding Bowel Cancer
Download our Understanding Bowel Cancer booklet to learn more.
Download now
Expert content reviewers:
A/Prof David A Clark, Colorectal Surgeon, Royal Brisbane and Women’s Hospital, and The University of Queensland, QLD, and The University of Sydney, NSW; A/Prof Siddhartha Baxi, Radiation Oncologist and Medical Director, GenesisCare Gold Coast, QLD; Dr Hooi Ee, Specialist Gastroenterologist and Head, Department of Gastroenterology, Sir Charles Gairdner Hospital, WA; Annie Harvey, Consumer; A/Prof Louise Nott, Medical Oncologist, Icon Cancer Centre, Hobart, TAS; Caley Schnaid, Accredited Practising Dietitian, GenesisCare, St Leonards and Frenchs Forest, NSW; Chris Sibthorpe, 13 11 20 Consultant, Cancer Council Queensland; Dr Alina Stoita, Gastroenterologist and Hepatologist, St Vincent’s Hospital Sydney, NSW; Catherine Trevaskis, Gastrointestinal Cancer Specialist Nurse, Canberra Hospital, ACT; Richard Vallance, Consumer.
Page last updated:
The information on this webpage was adapted from Understanding Bowel Cancer - A guide for people with cancer, their families and friends (2021 edition). This webpage was last updated in June 2021.