Page last updated: April 2024
The information on this webpage was adapted from Understanding Radiation Therapy - A guide for people with cancer, their families and friends (2024 edition). This webpage was last updated in April 2024.
Expert content reviewers:
This information was developed with help from a range of health professionals and people affected by cancer who have had radiation therapy:
- A/Prof Susan Carroll, Senior Staff Specialist, Radiation Oncology, Royal North Shore Hospital, and The University of Sydney, NSW
- Katie Benton, Advanced Dietitian Oncology, Sunshine Coast Hospital and Health Service, QLD
- Adrian Gibbs, Director of Physics, Radiation Oncology, Princess Alexandra Hospital Raymond Terrace, QLD
- Sinead Hanley, Consumer
- Dr Annie Ho, Radiation Oncologist, GenesisCare, Macquarie University Hospital and St Vincent’s Hospital, NSW
- Angelo Katsilis, Clinical Manager Radiation Therapist, Department of Radiation Oncology, Royal Adelaide Hospital, SA
- Candice Kwet-On, 13 11 20 Consultant, Cancer Council Victoria
- Jasmine Nguyen, Radiation Therapist, GenesisCare Hollywood, WA
- Graham Rees, Consumer
- Nicole Shackleton, Radiation Therapist, GenesisCare Murdoch, WA
- Dr Tom Shakespeare, Director, Cancer Services, Mid North Coast Local Health District, NSW
- Gabrielle Vigar, Nurse Lead, Cancer Program, Royal Adelaide Hospital and Queen Elizabeth Hospital, SA
External beam radiation therapy (EBRT) is the most common type of radiation therapy. It directs high-energy radiation beams at the cancer.
EBRT is delivered using a radiation machine. The most common type is a linear accelerator. You will lie on a treatment table or 'couch' under the machine.
The machine does'nt touch you, but will rotate around you to deliver radiation to the area with cancer from different directions. This allows the radiation to be more precisely targeted at the cancer and limits the radiation given to surrounding normal tissues.
The radiation beam is on for only a few minutes and you won't see or feel anything.
Common types of EBRT
EBRT can be given using different techniques and types of radiation. The radiation oncologist will recommend the most suitable method for you.
If you need a type of radiation therapy that is not available at your local hospital, they may arrange for you to have it at another centre.
Most machines use imaging scans before and during treatment to check you are in the correct position. This is known as image-guided radiation therapy (IGRT). It may use x-rays, a CT scan or an MRI scan.
- Three-dimensional conformal radiation therapy (3DCRT) – This is the basic form of modern EBRT using a LINAC. It shapes (conforms) the radiation beam to fit the treatment area.
- Intensity-modulated radiation therapy (IMRT) – This is a highly accurate type of conformal radiation therapy. It shapes and divides multiple beams of radiation into tiny beams (beamlets) to closely fit the tumour while healthy tissue nearby receives lower doses of radiation.
- Volumetric modulated arc therapy (VMAT) or rapid arc – This is a more advanced type of IMRT. As the machine moves around you, it reshapes and changes the intensity of the radiation beam.
- Stereotactic radiosurgery (SRS) and stereotactic radiation therapy (SRT) – These are specialised types of radiation therapy used for brain tumours, not a type of surgery. Many small beams of radiation are aimed at the tumour from different directions to target the exact shape of the tumour. It may be delivered by a different type of machine, such as a Gamma Knife or CyberKnife.
- Stereotactic body radiation therapy (SBRT) – Also known as stereotactic ablative body radiation therapy (SABR), this method combines many small beams of radiation from different angles to target the exact shape of the tumour. It may be delivered by a different type of machine, such as a Gamma Knife.
“The radiation therapy department was able to schedule sessions for first thing in the morning to fit in with my work schedule. The sessions were really quick and I was able to drive straight to work afterwards. As a working mum, being able to continue going to work was so beneficial … having the support of my colleagues was invaluable.” Annie
Linear accelerator (LINAC)
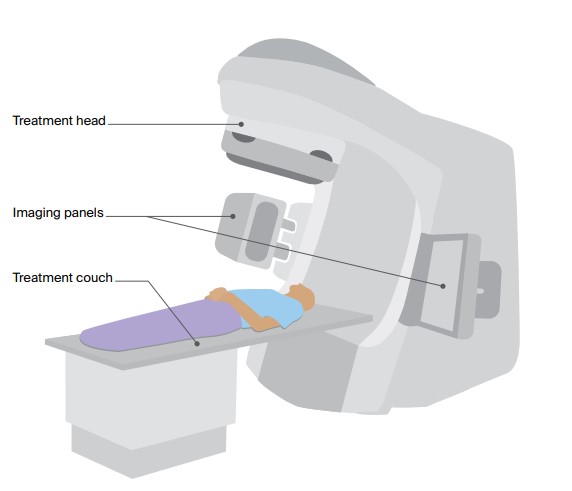
This is a general illustration of a LINAC, the most commonly used machine for delivering EBRT. The LINAC used for your treatment may look different.
A LINAC is large and often kept in a separate room. An imaging device, such as a CT imaging panel, is usually attached to the LINAC. This helps position you accurately on the couch so that the correct area of the body receives the radiation.
The radiation beam comes out of the treatment head, which moves around you while you lie still on the couch.
Planning EBRT treatment
EBRT needs to be carefully planned to ensure that enough radiation reaches the cancer, while as little radiation as possible reaches healthy tissues and organs. Planning may take place over a few appointments.
After the planning session, your radiation oncologist will work out the total dose of radiation needed and the total number of treatments.
This can take a few hours for urgent treatment or several days to weeks depending on your treatment needs.
Consultation session
- This may take up to two hours.
- To assess whether radiation therapy is the right treatment for you, the radiation oncologist will talk to you, do a physical examination, and look at all your test results and scans.
- They will explain how radiation therapy will help you, what will happen during planning and treatment, and what side effects to expect.
- You will also meet the radiation oncology nurse and a radiation therapist. They can provide support and further information. They will usually explain what side effects to expect and how to manage them.
- The radiation oncologist may arrange further x-rays, scans or other tests to find out more about the cancer.
- Consider taking someone with you to keep you company, ask questions and make notes.
- Ask what you will have to pay for treatment.
Planning (simulation) session
- This is usually done soon after the consultation session, and lets your treatment team work out how to direct the radiation and best position your body for treatment.
- You’ll have a planning scan which may be a CT, MRI or PET scan.
- You will have the planning scan in the same position you will be placed in for treatment.
- If you are having radiation to the chest area, you may need to hold your breath during the planning scan. You may also have a special CT scan, called a 4DCT, to track your breathing or be taught how to take deep breath holds.
- If you are having radiation therapy to the pelvic area, the size of your bladder and bowel will be checked during the scan. You may be asked to drink a set amount of water before each treatment session to make sure the bladder is full and the area having treatment is in the same position each time. You might also be asked to empty your bladder or bowel.
- The images are sent to a special computer that lets the radiation oncologist and radiation therapists work out how to direct the radiation.
Helping you keep still
- You may need some type of device to help you stay in exactly the same position for each treatment session and keep still for around 5-10 minutes.
- This is known as an immobilisation device. It will be made during the CT planning session. Depending on the area being treated, the device could be a breast board, a knee or foot cushion, or a bag that moulds to the shape of your body.
- For radiation therapy to the head or neck area, you may need to wear a plastic immobilisation mask. This will be made to fit you. A mask can feel strange and confining, but you will still be able to hear, speak and breathe.
- Some centres offer surface guided radiation therapy (SGRT). This uses special cameras to position you on the table and monitor your body’s movements during treatment. This means you won’t need an immobilisation device or skin markings.
Markers
- To make sure you are in the same position each session, a few permanent ink spots (tattoos) may be marked on your skin. These tattoos are the size of a small freckle and can’t be easily seen.
- Sometimes temporary ink marks are made on the skin. Ask the radiation therapists if you can wash these marks off or if need to keep them until the end of the treatment. The ink may be redrawn during the course of treatment, but it will gradually fade. Invisible tattoos may also be available.
- If you have to wear a mask or cast, the markings may be made on this device rather than on your skin.
- To help with image-guided radiation therapy, as well as tattoos you may have a surgical procedure to insert small markers (usually made of gold) into or near the cancer. These internal markers can be seen on scans during treatment.
What to expect at treatment sessions
You will usually start radiation therapy a few days or weeks after the planning session. your treatment team will let you know what time to arrive and how long you will need to be in the radiation therapy department.
There will be at least two radiation therapists at each treatment session. You may be asked to change into a hospital gown and remove any jewellery before you are taken into the treatment room.
After the treatment session you will see the radiation oncologist, a registrar (a hospital doctor training to be a radiation oncologist) or a radiation oncology nurse regularly to check your progress and discuss any side effects.
Positioning you for treatment
The treatment room may be in semi-darkness so the therapists can see the light beams from the treatment machine and line them up with the tattoos or marks on your body or mask.
After the radiation therapists position you on the treatment couch, they will leave the room to take some imaging scans using the imaging device attached to the treatment machine.
They will check the scans and make any adjustments needed to make sure you are in the same position as you were during the planning session. This may mean moving the table from outside the room or coming back into the room to move your body.
Receiving the treatment
Once you are in the correct position, the radiation therapists will control the treatment machine from a nearby room. They can see you on a television screen and you can talk to them over an intercom. The lights can be on during treatment.
The machine will move around you but it will not touch you. You won’t see or feel the radiation but you may hear a buzzing noise from the machine while it is working and when it moves.
The radiation therapists may turn off the machine and come into the room to change your position or adjust the machine.
It is important to stay very still to ensure the treatment targets the correct area. The radiation therapists will tell you when you can move. You will usually be able to breathe normally during the treatment. For treatment to some areas, such as the chest, you may be asked to take a deep breath and hold it while the radiation is delivered.
The treatment itself takes only a few minutes, but each session of EBRT may last around 10–40 minutes because of the time it takes the radiation therapists to set up the equipment, place you into the correct position and do the imaging scans.
The first session may take longer while checks are performed. You will be able to go home once the session is over.
Managing discomfort
EBRT itself is painless and you won’t feel it happening. If you feel some discomfort when you’re lying on the treatment table, tell the therapists – they can switch off the machine and start it again when you’re ready.
If you’re in pain because of the position you’re in or because of pain from the cancer, talk to the radiation oncology nurse. They may suggest you take pain medicine before each session.
Some people who have treatment to the head say they see flashing lights or smell unusual odours. These effects are not harmful, but tell the radiation therapists if you have them.
Taking safety precautions
EBRT does not make you radioactive because the radiation does not stay in your body after each treatment session. You will not need to take any special precautions with bodily fluids (as you would with chemotherapy).
It is safe for you to be with other people including children and pregnant women, and for them to come to the radiation therapy centre with you. However, they cannot be in the room during the treatment.
Managing anxiety before and during EBRT
The radiation therapy machines are large and kept in an isolated room. This may be confronting, especially at your first treatment session.
You may feel more comfortable as you get to know the staff, procedures and other patients.
Wearing an immobilisation mask may make you feel anxious or claustrophobic before or during treatment, and if this happens you should tell the radiation therapists.
With the support of the radiation therapy team, many people find that they get used to wearing the mask.
The team may suggest you try breathing or relaxation exercises, or listening to music to help you relax. A mild sedative may also help.
Learn more
Specialised types of EBRT
Total body irradiation (TBI)
A form of radiation therapy given to the whole body for blood cancers. Sometimes TBI is given with chemotherapy to prepare people for a stem cell or bone marrow transplant.
You will be admitted to hospital to have TBI. A course of TBI may be given as one dose or as several doses over a few days. Your treatment team will talk to you about your treatment schedule and any side effects you may have.
Proton therapy
This uses radiation from protons rather than x-rays, which release most of their radiation within the cancer. This is different to standard EBRT beams, which pass through the area and nearby healthy tissue.
Special machines called cyclotrons and synchrotrons are used to generate and deliver the protons. Proton therapy may be useful when the cancer is near sensitive areas, such as the brain stem or spinal cord.
Proton therapy is not yet available in Australia (as at March 2024), but there is government funding to allow Australians with specific cancer types to travel overseas for treatment. Your radiation oncologist can advise if you are eligible and provide more details.
A centre to deliver proton therapy in Australia is under construction. When complete, the Australian Bragg Centre for Proton Therapy and Research in Adelaide will treat some childhood and rare cancers.