Page last updated: January 2024
The information on this webpage was adapted from Breast Prostheses and Reconstruction (2023 edition). This webpage was last updated in January 2024.
Expert content reviewers:
- Dr Jane O’Brien, Specialist Oncoplastic Breast Cancer Surgeon, St Vincent’s Private Hospital, VIC
- Clare Bradshaw, Clinical Nurse Consultant, Breast Assessment Unit, Fiona Stanley Hospital, WA
- Rene Hahn, Consumer
- Sinead Hanley, Consumer
- Dr Marc Langbart, Specialist Plastic and Reconstructive Surgeon, Randwick Plastic Surgery, NSW
- Melanie Law, Consumer
- Sally Levy, Consumer
- Annmaree Mitchell, Consumer
- Ashleigh Mondolo, Breast Cancer Nurse Clinical Consultant, Mater Private Hospital Brisbane, QLD
- Rochelle Osgood, Clinical Nurse Consultant – McGrath Breast Care Nurse, Sunshine Coast University Hospital, QLD
- Dr Kallyani Ponniah, Head of Department, Breast Centre, Sir Charles Gairdner Hospital, WA
- Meg Rynderman OAM, Consumer
- Sarah Stewart, Breast Care Nurse, The Royal Women’s Hospital, VIC
- Erin Tidball, 13 11 20 Consultant, Cancer Council NSW
- Jane Turner, Senior Exercise Physiologist, Sydney Cancer Survivorship Centre, Concord Cancer Centre, NSW.
This page provides information about having a breast reconstruction after breast cancer surgery. For information about breast cancer and what to expect before, during and after surgery, see Understanding breast cancer and Understanding surgery.
It's estimated that almost one in three women in Australia has a breast reconstruction after a mastectomy.
Key questions
When can I have a reconstruction?
Breast reconstruction can be done at the same time as a mastectomy (immediate reconstruction) or months or years later (delayed reconstruction). The timing depends on the type of breast cancer you were diagnosed with, whether you need further treatment (for example, chemotherapy or radiation therapy), the type of reconstruction, your general health, and other concerns, such as the cost.
Immediate reconstruction
If you have a breast reconstruction during the mastectomy, it may be possible to save most of the skin but not the nipple (skin-sparing mastectomy). Sometimes it may be possible to leave the nipple in place (nipple-sparing mastectomy). Having a skin- or nipple- sparing mastectomy often means a more natural look and fewer scars.
Delayed reconstruction
Sometimes you won’t be able to have an immediate reconstruction because of medical and cancer treatment or the surgery schedule at the hospital. You may also need to have the reconstruction in a number of stages to achieve the desired result. Talk to your surgeon about these issues.
Who will do the reconstruction?
Breast reconstruction is done by a breast surgeon or a reconstructive (plastic) surgeon. If a breast surgeon is trained in plastic surgery, they are known as an oncoplastic breast surgeon.
The breast surgeon and the reconstructive (plastic) surgeon may do the breast cancer surgery and reconstruction during the same operation. A breast surgeon can do implant reconstructions and a reconstructive (plastic) surgeon can do both implant and flap reconstructions.
You can ask your surgeon:
- what the surgery will involve and the length of the recovery
- about their experience and expertise
- what risks are associated with the different types of reconstructions
- to show you photographs of their work, including how the reconstruction looks straight after surgery and several months later.
Finding a surgeon
When considering having a reconstruction, ask to be referred to an expert in breast reconstruction. Check that the breast surgeon is a member of Breast Surgeons of Australia and New Zealand (BreastSurgANZ) and that the reconstructive (plastic) surgeon is a member of the Australian Society of Plastic Surgeons.
Health professionals you may see
In hospital, you will be cared for by a range of health professionals who specialise in different aspects of a reconstruction procedure. Specialists and other health professionals will take a team-based approach to your care as part of a multidisciplinary team (MDT). The health professionals listed in the table below may be in your MDT.
| Health professional |
Role |
| breast surgeon |
performs breast surgery and biopsies; some breast surgeons also perform breast reconstruction |
| oncoplastic breast surgeon |
performs breast surgery and biopsies; performs some types of breast reconstruction |
| reconstructive (plastic) surgeon |
uses a variety of plastic surgery techniques to reconstruct the breast’s appearance after surgery |
| anaesthetist |
assesses your health before surgery; administers anaesthesia and looks after you during the surgery; commonly plans your pain relief after surgery |
| breast care nurse |
assesses your health before surgery; administers anaesthesia and looks after you during the surgery; commonly plans your pain relief after surgery |
| radiation oncologist |
treats cancer by prescribing and overseeing a course of radiation therapy |
| medical oncologist |
treats cancer with drug therapies such as chemotherapy, targeted therapy and immunotherapy |
| occupational therapist, physiotherapist |
links you to support services and helps you with any emotional, practical and financial issues |
| social worker |
links you to support services and helps you with any emotional, practical and financial issues |
| counsellor, psychologist, clinical psychiatrist |
help you manage your emotional response to diagnosis and treatment |
What to do before surgery
Stop smoking or vaping – If you smoke tobacco or vape, aim to quit as soon as possible. Continuing to smoke or vape can damage the blood vessels and increase the risk of complications after surgery. This can delay skin healing and recovery time. For support, talk to your doctor or call the Quitline on 13 7848.
Exercise regularly – This will help you build up your strength to cope with recovery and reduce the risk of complications after surgery. Talk to your doctor, physiotherapist or exercise physiologist about the amount and type of exercise that is right for you.
Talk to someone – It’s natural to feel anxious before surgery. Talk to your treatment team, or call Cancer Council 13 11 20 to arrange to speak to a trained Cancer Connect volunteer who has had reconstruction surgery and can offer you support.
Types of breast reconstruction
The main types of breast reconstruction are implant reconstruction or flap reconstruction, or a combination of the two.
Most reconstructions involve two or more operations. Your reconstructive surgeon will discuss the different methods and suggest the most suitable one for you.
Your reconstruction options will depend on several factors:
- your preference
- your body shape and build, and whether you have a body mass index (BMI) over 30
- your general health
- the surgeon's experience
- how much breast tissue has already been removed
- any scars or previous operations to the area of your body where tissue will be taken
- the quality of the remaining skin and muscle
- the breast size you would like
- whether one or both breasts are affected
- whether you need radiation therapy or have already had it
- whether you smoke or vape or have recently quit - this can affect the type and timing of the reconstruction you can have.
Implant reconstruction
An implant is a sac that's filled with either silicone gel or saline to create a breast shape. You may have an implant reconstruction as a one-stage or two-stage operation.
In the one-stage operation, the surgeon puts in a permanent implant during the mastectomy. In the two-stage operation a tissue expander is used to inflate and stretch the skin so there is room for the implant.
After the reconstruction you will have a scar on your breast. The type of scar will depend on the type of cut (incision) that your breast and reconstructive (plastic) surgeons choose.
Types of implants
All implants are made with an outer layer (shell) of silicone. They can be filled with silicone gel or saline (salt water).
Silicone gel implants
These are used in almost all implant reconstructions. A softer, honey-like type of gel was previously used, but implants are now made of a soft, semi-solid filling called cohesive gel. This gel is quite firm and holds its shape like jelly.
The surface of these implants can feel smooth (micro textured) or have a rough surface (macro textured). Textured implants grip to tissue better and are less likely to move position than smooth implants.
Saline implants
These are no longer commonly used in reconstruction. Saline breast implants don't look and feel as natural as silicone implants. They may wrinkle under the skin and may leak, leading the implant to deflate and require replacement.
What to consider – implant reconstruction
|
|
Benefits
|
Drawbacks
|
- Operation takes only a few hours and you usually only stay in hospital for a few days.
- Creates the breast shape without moving tissue (muscle, skin or fat) from elsewhere in the body, so these parts aren't affected.
- Only one scar from the mastectomy.
- Recovery time at home is shorter than for a flap reconstruction. Although the chest area will be swollen and sensitive, you may be able to return to most activities after four weeks (no heavy lifting for six to eight weeks).
- Implants come in a range of shapes and sizes. You can choose to change your original breast size.
- Doesn't usually cause muscle weakness, only temporary discomfort and pressure.
- May make you more confident when naked.
|
- May not be suitable if you plan to have radiation therapy.
- Two or more operations may be required if you have an expander first. You will need regular doctor's visits to gradually fill the expander, which may take 3–6 months.
- A breast reconstructed with a tissue expander usually feels firm and doesn't move like the original breast, but it usually looks the same in a bra.
- If your other breast changes in shape and size, you may need further surgery to match the two.
- Hardened scar tissue (capsule) may form around the implant. This can change the shape of the breast and may be painful.
- Risk of infection, which may mean removing the implant.
- Implants may eventually need to be replaced.
- Some rare side effects (see below).
- Increased risk of lymphoedema.
|
How an implant reconstruction is done
One-stage operation
This operation is sometimes called a direct-to-implant reconstruction. It is usually done at the same time as a skin- or nipple-sparing mastectomy, when there is enough tissue left on the chest to cover the implant. The surgeon can place the implant above or under the chest (pectoralis) muscle.
| Subpectoral implant reconstruction |
Prepectoral implant reconstruction |
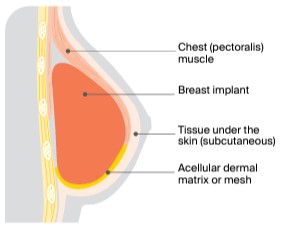 |
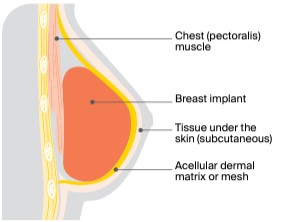 |
| The breast implant is placed under the chest muscle. The lower and outer part of the implant is often covered by a material called dermal matrix or mesh to hold the implant in place. |
The breast implant is placed in front of the chest muscle, directly under the skin and the layer of tissue just under the skin. The whole outer part of the implant is covered by a dermal matrix or mesh to hold the implant in place. |
Two-stage operation
Tissue expansion is a process that stretches the remaining chest skin and soft tissue to fit the breast implant. This is done in two stages. The two-stage approach is often used when radiation therapy is given after a mastectomy and before the implant is put in.
| First stage: Implanting the tissue expander |
Second stage: Expanding the tissue expander |
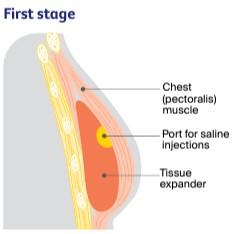 |
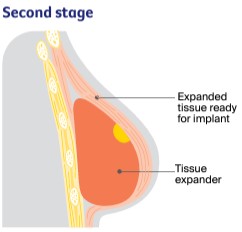 |
| A balloon-like bag called a tissue expander is placed under or in front of the chest muscle. Every couple of weeks, the balloon is injected with saline through a port (a thin tube). You may be given 1–6 injections depending on how much the skin and muscle need to stretch. The stretched tissue creates a pocket for the breast implant. The saline injections are usually not painful. |
The tissue stretches and expands each time saline is added. You may feel discomfort for a few days. When the expander has stretched the tissue enough, you have a second operation to remove the temporary expander and insert the implant in its place. You may need to stay in hospital overnight after this second operation. |
Risks of having an implant reconstruction
Before the operation, the surgeon will discuss the risks of an implant reconstruction with you. These may include:
- Infection - You'll be given antibiotics at the time of the operation to reduce the risk of infection. But if this happens, the implant may have to be removed until the infection clears. The implant can then be replaced with a new one.
- Implant rupture - Implants can leak or break (rupture) because of gradual weakening of the silicone over time. A rupture is not harmful to your body, but you will need to have surgery to remove the empty silicone envelope and replace the implant. Implants need to be regularly examined, and may need to be changed every 10-15 years.
- Hardening of the implant - A fibrous covering can form around a breast implant, which can make the breast feel firm if it hardens over time. This is called capsular contracture, and it is more common after radiation therapy. Further surgery may be needed to remove and/or replace the implant. A new surgical procedure call capsulotomy can be done to loosen the scar tissue surrounding the implant.
- Movement - The position of the implant in the body may change slightly over time. This is called implant malposition, displacement, descent or rotation. Further surgery can restore the implant to its original position if it shifts a lot.
- Visible rippling - Sometimes implants adhere to the surface of the skin and this can affect how smooth the breast is. This can often be corrected with minor surgery called lipomodelling.
- Lymphoma - There have been reports of a link between textured breast implants and a rare type of non-Hodgkin lymphoma known as breast implant associated anaplastic large cell lymphoma, or BIA–ALCL. BIA–ALCL is a cancer that grows in the fluid and scar tissue that forms around a breast implant. The Therapeutic Goods Administration (TGA) recommends monitoring your breasts for any changes such as swelling, a lump or pain ( learn more). The TGA also has an online breast implant hub, where information and support related to breast implants and their safety are updated as new evidence becomes available.
- Other health problems - Research has not established that silicone breast implants cause autoimmune disorders such as scleroderma, rheumatoid arthritis or lupus. There is also no evidence that implants cause breast cancer.
Staying informed about the safety of your implants
While implants are generally considered to be safe, there have been some concerns about risks.
Some silicone implants were voluntarily taken off the market in the 1990s due to safety concerns. Since then, regulatory authorities such as the Therapeutic Goods Administration (TGA) must approve brands used in Australia.
In late 2019, the TGA removed from sale some textured breast implants. The TGA also imposed extra conditions on other implants due to concerns over BIA-ALCL.
The Australian Breast Device Registry (ABDR) is a national clinical quality registry for all people having breast implant surgery. The aim of the registry is to provide a way to track the long-term safety and performance of breast implants. This can help identify early signs of problems with a device.
ABDR is supported by the Australian Society of Plastic Surgeons, Breast Surgeons of Australia & New Zealand and Australasian College of Cosmetic Surgery and Medicine. Your surgeon will provide you with printed information about the registry and you'll be contacted by ABDR after the surgery with more information.
Flap reconstruction
The shape of a breast can be built using your own muscle, fat and skin from another part of the body. This is called a flap or autologous reconstruction.
Your surgeon will discuss the type of flap reconstruction that is most suitable to you, which may depend on if you have large breasts, don't have enough skin to cover an implant, or have had radiotherapy. This type of reconstruction may not be suitable if you smoke, have diabetes, connective tissue disease or vascular disease, have had previous major abdominal surgery, or have a higher BMI.
“Because I’d had extensive radiation therapy to the chest area, I was only suitable for a flap reconstruction. My reconstructed breast is absolutely amazing. It’s very symmetrical and even.” LESLEY
What to consider – flap reconstruction
|
|
Benefits
|
Drawbacks
|
- Reconstruction is permanent once the breast has healed.
- Most methods only use your own living tissue to create the breast. This often gives a better match to the other breast, which may be important to you.
- The flap maintains its look and feel over the long term and generally adjusts if your body's weight changes.
- Using your own tissue means there is no risk of possible rupture.
- Less chance of long-term complications.
- Less likely to need further surgery in the future.
- May make you more confident when naked.
|
- Flap reconstruction is more extensive than implant reconstruction, and additional treatment or follow-up surgeries are sometimes needed. The operation will take several hours and you may need to stay in hospital for about a week.
- Recovery takes longer than after an implant reconstruction as there is a wound at the site where the flap was taken as well as a breast wound to heal.
- Risks include infection and the flap not healing properly.
- Surgery usually causes more than one scar (but these fade).
- Depending on the type of flap, you may also need an implant.
- TRAM and DIEP procedures can only be done once.
- There is a small risk of hernia with abdominal flaps.
|
Location of flap reconstruction
Flap from the lower abdomen (DIEP or TRAM)
Tissue from the lower abdomen (tummy) is used to reconstruct the breast shape. There are 2 main types of abdominal flaps: free deep inferior epigastric perforator (DIEP) flap, and free transverse rectus abdominis myocutaneous (TRAM) flap. These flaps are called free flaps because the flap is cut completely away from the blood supply in the abdomen. The surgeon then reconnects the flap to the blood vessels in the chest area using microsurgery (surgery using miniature instruments and viewed through a microscope).
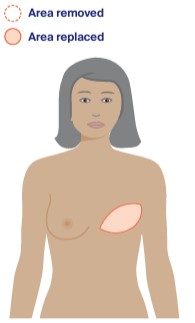
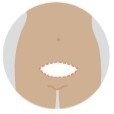
DIEP flap reconstruction
This is called DIEP because it uses deep blood vessels called deep inferior epigastric perforators (DIEP). It is now done more often than TRAM flap procedures. In a DIEP flap procedure, the surgeon uses only the skin and fat to reconstruct the breast. The abdominal muscle is left in place. This means the strength of your abdomen muscle is less affected and the risk of abdominal problems after surgery is reduced.
TRAM flap reconstruction
In this procedure, all or some of the muscle in the lower abdomen and a flap of skin and fat are used to reconstruct the breast shape. The muscle in the lower abdomen that runs from the breastbone to the pubic bone is the rectus abdominis muscle, or “six pack” muscle. A type of TRAM flap reconstruction that is not often done anymore is called a pedicle TRAM flap. In this procedure, the flap remains attached to its original blood supply and is tunnelled under the skin of the upper abdomen to the breast. A pedicle TRAM flap has a high risk of hernia.
How the abdomen will look after reconstruction
After a DIEP or TRAM flap reconstruction, your abdomen is tighter and flatter. This is because the reconstructed breast is formed from tissue taken from the abdominal area.
You will have a long scar across the lower abdomen from one hip to the other, a scar around your bellybutton and a scar on the reconstructed breast. While everyone heals differently, the appearance of the scars will improve with time.
Both types of flap reconstructions can make the abdominal area weaker, and you will have little to no feeling in the skin over the breast and the scar over the abdomen. You may be advised to wear a garment called an abdominal binder to protect and support the wound. Ask your surgeon how long you will have to wear the binder.
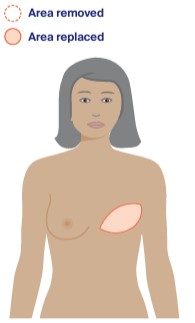
Flap from the back (LD flap reconstruction)
The latissimus dorsi (LD) is a muscle on the upper back that controls shoulder movement. This muscle and some skin and fat can be moved from the back around to the chest to reconstruct the breast shape.
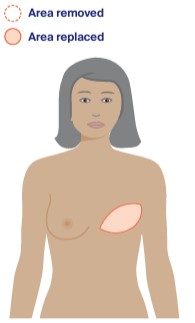

This reconstruction can be completed in one operation, but the surgeon will usually place an implant under the flap to create a breast that is similar in size to your remaining breast. If you have a tissue expander, the surgeon will begin the expansion process after the flap has healed. Unless you have a nipple-sparing mastectomy, the areola and nipple are created in a separate operation.
The size of the scar on the back will depend on the surgeon – most times it can be hidden by a bra strap. The scar on the breast will vary depending on the type of mastectomy you had.
A new technique avoids a scar on the back by reopening the mastectomy scar and then special instruments are inserted to bring the latissimus dorsi muscle forward towards the breast. This surgery is now widely available. Ask your surgeon if this is suitable for you.
Less common flap reconstructions
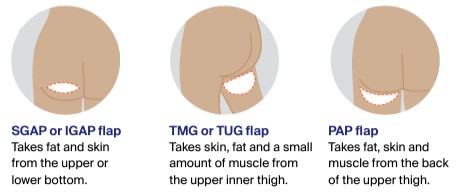
If a DIEP, TRAM or LD flap is not suitable, you may be offered reconstruction techniques that use fat and a blood supply from another area of the body. These include:
- superior gluteal artery perforator (SGAP) flap or inferior gluteal artery perforator (IGAP) flap using tissue from the bottom
- transverse myocutaneous gracilis (TMG) flap, transverse upper gracilis (TUG) flap or profunda artery perforator (PAP) flap using tissue from the inner thigh.
To help reconstruct a small breast shape, the surgeon may remove fat from another part of the body (liposuction), then inject it into the breast to create or improve the shape and contour.
Risks of having a flap reconstruction
Before the operation, the surgeon will discuss the risks of a flap reconstruction with you. Some of these risks include:
- Loss of the flap - Blood vessels supplying the flap may kink or get clots, leading to bleeding and a loss of circulation. If there are signs of problems with the blood supply, you might need another operation. If the blood supply is not good enough, this may cause the tissue to die, leading to a partial or complete loss of the flap. Problems with blood supply are more likely to happen if you smoke or have recently quit or are carrying extra weight. If the flap dies, you usually have to wait 6–12 months before having a reconstruction again.
- Hardening of the flap - In rare cases, the fat used to make a TRAM or DIEP flap doesn’t get enough blood supply and dies. This is known as fat necrosis. Because it causes the affected area in the reconstructed breast to feel hard, fat necrosis can easily be seen and diagnosed on a mammogram. It can be left in place or surgically removed, and is more likely to happen if you smoke or have had radiation therapy.
- Problems with the donor site - After an abdominal flap reconstruction, it may take time for the wound to heal, and fluid can collect (seroma) in the abdominal region. After an LD flap reconstruction, it’s common for fluid to build up (seroma) in the back where the muscle was taken from.
- Hernia (abdominal bulge) - If you have had a DIEP or TRAM flap, you have a small risk of developing a hernia. A hernia occurs when part of the bowel sticks through a weak point in the abdominal wall. The risk of an abdominal hernia is greater with a TRAM flap than with a DIEP flap reconstruction because removing the TRAM flap can weaken the abdominal wall and cause a hernia.
Re-creating the nipple
You may only want the shape of the breast reconstructed, others choose to have the look of a nipple. The appearance of the nipple and areola can be created in several ways.
Adhesive nipples
These stick to the skin or breast prosthesis and stay in place for several days. They are made from soft silicone and are available in a variety of colours. You can buy them from breast prostheses suppliers.
Nipple made from your own body tissue
A small operation can reconstruct a nipple and the areola. This operation is generally done a number of months after a reconstruction to give your body time to heal from the original operation and because the reconstructed breast may drop slightly after surgery.
The nipple is made from tissue on your reconstructed breast. It is folded to create a nipple shape. The new nipple won’t have nerves, so it will not feel any sensation or become erect to touch. Sometimes the nipple can flatten out and sometimes it can be permanently erect.
Nipple tattoo
The new nipple can be tattooed to match the colour of the other nipple. The tattoo can be done by a reconstructive (plastic) surgeon, trained nurse, professional medical tattooist or specially trained cosmetic therapist. Initially, the tattoo will look darker than the remaining nipple, but it will fade with time to match in colour.
A new technique called 3D nipple tattoos uses different shading to create the appearance of a nipple. Your breast care nurse can give you more information about this new procedure.
Surgery to the other breast
Often the difference between the remaining and the reconstructed breast is small and not noticeable when wearing a bra. But if the difference in breast size is more obvious, you may decide to have the remaining breast made smaller or larger through surgery to match the reconstructed breast and improve balance and posture.
Bilateral mastectomy
You may be advised or choose to have a bilateral mastectomy, also called a double mastectomy. This means both breasts are removed at the same time. A bilateral mastectomy may be recommended because of:
- the type of breast cancer you have
- your risks and/or anxiety about developing another breast cancer
- family history or a gene fault that increases your breast cancer risk
- the amount of surgery required to achieve a symmetrical result with the breast reconstruction
- choosing an abdominal flap reconstruction, as surgery on the abdomen can only be done once (can't be repeated at a later date if cancer develops in the other breast).
Reconstruction or going flat will need to be considered for both breasts. Discuss this issue with your doctor and seek a second opinion if you wish.
Therapeutic mammaplasty
This procedure combines surgery to treat breast cancer with surgery to reduce the size of the breast. It is often used as an alternative to mastectomy in suitable cases. Sometimes a breast reduction is done on the other breast at the same time, or at a later date.
What to expect after a reconstruction
Everyone reacts to surgery differently, and the type of surgery you've had will influence the side effects you have.
Short-term effects
Appearance of the breast
It’s common to feel nervous when the bandages and dressings are first removed. It will take time for the bruising and swelling to fade, and the appearance of a breast reconstruction using a tissue flap may take longer to settle. If you’re disappointed with the appearance of the breast, you may have other operations or procedures to improve the look and shape of the breast.
Pain relief
After any type of operation, you will be given pain medicines to ease your discomfort. You will also probably have small tubes (drains) inserted into the operation site to remove excess fluid, and may go home with them. If you have had a flap reconstruction, you will be sore in the area where the other tissue and/or muscle were taken, as well as in the breast area.
Healing problems
Sometimes the area will not heal well within the first week or so after surgery. This can be caused by infection, poor blood supply or problems with an implant or flap. Any infection must be treated to reduce the possibility of further complications. If an implant has been used, it might need to be taken out. It may be possible to have a new implant put in at a later date.
Bleeding
Blood may build up in or under the wound. This is called a haematoma, and it causes swelling and pain. A large haematoma may need to be removed by surgery.
Seroma
In some cases, when drains have been removed, extra fluid collects in or under the wound. This is called a seroma, and it causes swelling and pain. It may need to be removed by a health professional using a needle. You can wear a special bra called a compression bra to help relieve the pain.
Scars
All types of breast reconstruction will leave a scar. Everyone heals differently, and the final appearance of a scar will vary, even if the surgery is the same. Most scars have a thickened, red appearance at first, but they will usually fade after about 3 months.
Sometimes the scar stays thick and becomes itchy and uncomfortable. Before the surgery, let your surgeon know if you have other raised, irregular scars (sometimes called keloid scars), as this may show that you are prone to getting these types of scars. Your surgeon or breast care nurse can advise you about treatments to reduce the discomfort. You may be able to have further surgery to improve the scar’s appearance.
Long-term considerations
Pregnancy
Breast reconstruction doesn’t affect your ability to become pregnant or carry a baby. There is a small risk of having a hernia during pregnancy if you had an abdominal flap reconstruction. Your doctor will talk to you about any risks you may have and how to manage them.
Breastfeeding
It will not be possible to breastfeed with the reconstructed breast. You may be able to breastfeed successfully with the other breast, although this may be difficult if you have had reduction surgery in this breast. You can ask a breast care nurse or lactation consultant any questions you have about breastfeeding after a reconstruction.
Taking care of yourself after a reconstruction
How long your recovery takes will depend on your age, general health and the type of surgery you had.
- Rest - When you get home from hospital, you will need to take things easy for the first few weeks. Ask family and friends to help you with chores so you can rest.
- Driving - You will probably need to avoid driving for 4–6 weeks after surgery. Discuss this timing with your breast surgeon.
- Lifting - Avoid repetitive arm movements (e.g. hanging out washing, vacuuming), heavy lifting (more than 5 kg, so this may include shopping bags) and activities that strain your arm. You can gradually return to your usual activities after 4–8 weeks.
- Tummy problems - After abdominal flap surgery, you may have weaker abdominal muscles. Get up from a low chair or sit up in bed carefully. Wearing supportive underwear will help. If the weakness continues after 6 weeks, ask your doctor for a referral to a physiotherapist or an exercise physiologist for an exercise program.
- Loose clothing - Until the area is healed, wear loose fitting comfortable clothing.
- Follow-up appointments - Continue to see the specialist who performed the reconstruction until your body has healed.
Costs and financial assistance
Before you have surgery, find out how much it will cost to have a breast reconstruction. Check with your surgeon, the hospital, Medicare and your private health fund, if you have one, before deciding to go ahead. Find out whether you may need to pay for extras such as pain medicines, post-surgical bras and check-ups with your surgeon.
There are many services available for help with other costs associated with a reconstruction, such as transport costs to specialist medical appointments and the cost of accommodation. Ask the hospital social worker which services are available in your local area and if you are eligible to receive them.
If you need legal or financial advice, you should talk to a qualified professional about your situation. Cancer Council offers free legal and financial services in some states and territories for people who can't afford to pay – call 13 11 20 to ask if you are eligible.
If you have your nipple tattooed by a health professional with a Medicare provider number, it is covered by Medicare. If you have private health insurance, it may cover the cost of the tattooing.
"With my private insurance, I was significantly out of pocket. However, the advantage gained with the reconstruction was well worth the cost." – Gwen
What to consider – reconstruction costs
|
|
Public hospital
|
Private hospital
|
- Reconstruction after a mastectomy is a medical procedure, not a cosmetic one, so the costs are covered through Medicare for a public patient in a public hospital.
- There may be some extra charges if an implant is used.
- There may be some extra charges for private patients who have a reconstruction in a public hospital.
- If you choose to have a delayed reconstruction, you will be put on the hospital's elective surgery waiting list. Ask your surgeon about the likely waiting period.
- You can change your mind and decide not to proceed with the reconstruction even if you are on a waiting list.
|
- Private patients may be covered by their private health insurance or may have to pay the cost themselves.
- In a private hospital, Medicare will cover some of the surgeon's and anaesthetist's fees. Your health fund may cover some or all of the remaining costs, but you may need to pay a gap fee or a hospital admission fee.
- Part of or the entire cost of an inflatable tissue expander and any permanent implant may also be covered by your insurance provider.
- If you decide to join a health fund before your operation, you will have to wait the qualifying period before you can make a claim. This may be up to 12 months. Check with the different health funds.
- See Financial cost of cancer for more information.
|
Question checklist
You may find this checklist helpful when thinking about the questions you want to ask your breast or reconstructive (plastic) surgeon. If you don't understand the answers from the surgeon, it is okay to ask for clarification.
- Do you think I can have a reconstruction?
- When would you advise me to have the reconstruction?
- What types of reconstructions are suitable for me?
- If I need radiation therapy, will this affect the reconstruction or the type of reconstruction I can have?
- Will you do my reconstruction?
- What are the risks and possible side effects of this type of reconstruction?
- Do you specialise in this type of surgery?
- How long will I have to wait to have the reconstruction?
- Where can I have this surgery?
- How long will I need to stay in hospital? How long will my recovery take?
- How much will it cost? Are there any out-of-pocket expenses not covered by Medicare or my private health cover?
- How will the reconstructed breast look and feel?
- Can you show me photos of previous reconstructions you’ve done?
- Can I talk to others who have had a similar operation?
- Will the reconstruction hide any new problems? Do I still need regular mammograms?
- How can I get a second opinion?
- Who should I contact if I have questions or a problem after surgery?
- If there are complications, is it likely I’ll need more surgery?
Breast Prostheses and Reconstruction
Download our Breast Prostheses and Reconstruction booklet to learn more and find support.
Download now Order for free