
Blood cancers are uncommon. But Natasha knows how devastating they can be.
When the Melbourne nurse noticed unusual bruising on her body in January 2018, her daughter urged her to get checked.
It’s lucky she did: tests confirmed Natasha, a mother of two, had Acute Lymphoblastic Leukaemia (ALL), a rare cancer diagnosed in fewer than 200 adults in Australia each year.
“It was a shock,” Natasha said.
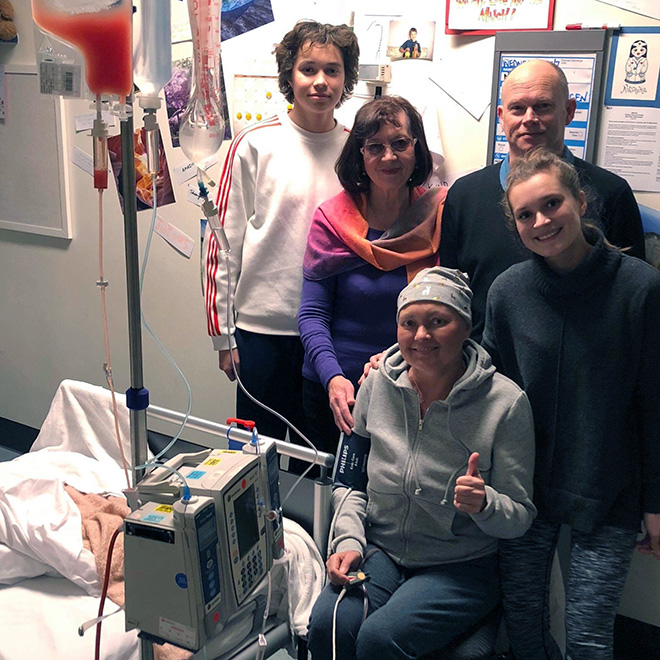
Natasha with her family in hospital during treatment
Sadly, the shock of a blood cancer diagnosis hits many people in Australia every year. This year, Australian Government data suggests around 18,000 people will be diagnosed with a blood cancer, which includes leukaemia, lymphoma and multiple myeloma. More than 4,000 of those diagnosed will be in Victoria and will feel the same shock and devastation that Natasha experienced.
Fortunately, thanks to your support, a renewed research focus in recent years is ensuring these low-survival cancers are not forgotten.
Understanding how blood cancers form
Crucial to combatting blood cancers is understanding their cause. Between 2017 and 2019, A/Professor Carl Walkley and his team were focused on learning how common mutations in patients with myelodysplastic syndromes (MDS) and related blood cancers cause these cancers.
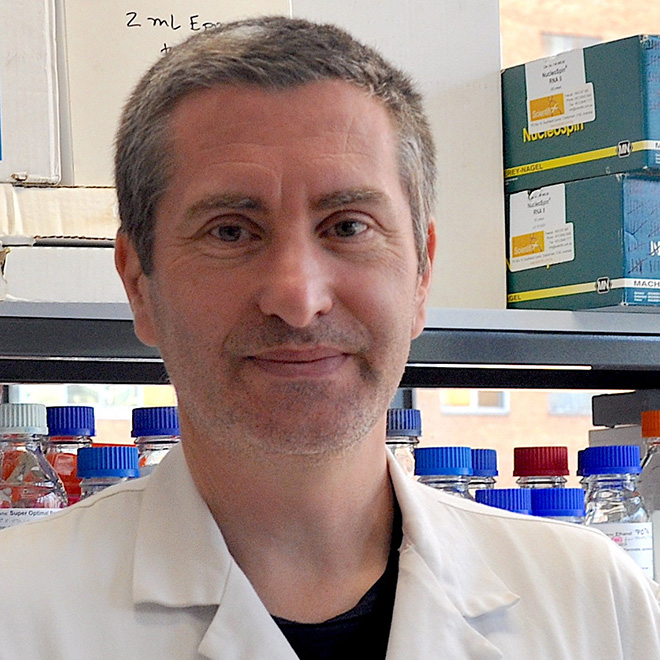
Associate Professor Carl Walkley
MDS are a group of blood cancers affecting the production of normal blood cells in our bone marrow.
The team developed a successful model showing that a common mutation in a gene called SRSF2 can cause MDS and related cancers to develop. While this has been modelled before, the one made by A/Prof Walkley and team most closely mirrors the development of these diseases in humans.
“This is extremely important as the aim of these studies is to generate models that match the human disease as closely as possible, and to then use these for identification, testing and evaluation of new treatments,” A/Prof Walkley, from St Vincent’s Institute of Medical Research, said. “Our model does this better than any other model worldwide.”
A/Prof Walkley hopes to continue this work to push towards better treatment for MDS and related cancers.
“We will use cells from these models to undertake screens for new ways to treat these cancers and prioritise new therapies for these currently poorly treated cancers,” A/Prof Walkley said.
MDS is a very rare cancer, with just 597 cases in Victoria in 2019. But A/Prof Walkley’s work will also be applicable to other types of blood cancer, like myeloproliferative neoplasms and types of leukaemia.
And, as people like Natasha know, progress against any of the numerous types of rare blood cancers can mean an incredible amount to those affected by them and their families – and this progress is thanks to your support.
A/Prof Walkley’s project ended in 2019. This year, a new project, focusing on leukaemia and lymphoma, began – with your help.
Targeting immune cells to treat leukaemia and lymphoma
Dr Daniel Utzschneider and his research team are studying the roles of T cells – an important part of our immune systems – in preventing the growth of tumour cells. These T cells often experience functional impairments known as ‘exhaustion’, affecting their ability to combat the cancer. However, Dr Utzschneider has discovered a subset of exhausted T cells that respond to immunotherapy.

By studying exhausted T cells responding to chronic lymphocytic leukaemia (CLL), he hopes to identify the factors limiting T cell functioning, and use them as novel therapeutic targets to improve T-cell immunity.
Dr Utzschneider hopes this will lead to improved outcomes for people affected by leukaemia and lymphoma. His team aims to find new ways to help T cells stand up against malignancies in the blood.
“The human immune system is very powerful in eliminating malignant cells,” he said. Understanding how to use it to its full potential can lead to tremendous outcomes for millions of patients.”
These outcomes, which Cancer Council supporters like you help create, change the lives of so many people – like Natasha.
After a difficult struggle, which involved six months of intense chemotherapy, a bone marrow transplant and the loss of her hair, Natasha went into remission and began to slowly recover from her experience.
“I’m getting there,” she said. “I’m starting to feel a bit more lifted up!”
And thanks to research like that of A/Prof Walkley and Dr Utzschneider, more people every year are seeing better outcomes after a blood cancer diagnosis. Since 1993, survival rates for ALL, which Natasha had, and CLL, the focus of Dr Utzschneider’s work, have risen by 20%.
A/Prof Walkley’s focus of MDS has seen a 16% survival increase in that time, while chronic myeloid leukaemia (CML) has seen an extraordinary 49% rise since then.
This is incredible progress against these traditionally low-survival and forgotten cancers. With the help of kind supporters like you, these amazing efforts will continue, ensuring more people like Natasha survive a blood cancer diagnosis.